Acute Kidney Injury (AKI) doesn’t announce itself with a siren. It creeps in quietly-maybe after a bad bout of food poisoning, a fall in blood pressure during surgery, or even after taking a common painkiller. One day, your kidneys are working fine. The next, they’re struggling to keep up. This isn’t chronic disease. This is sudden, dangerous, and often reversible-if you catch it in time.
What Exactly Happens When Your Kidneys Shut Down Suddenly?
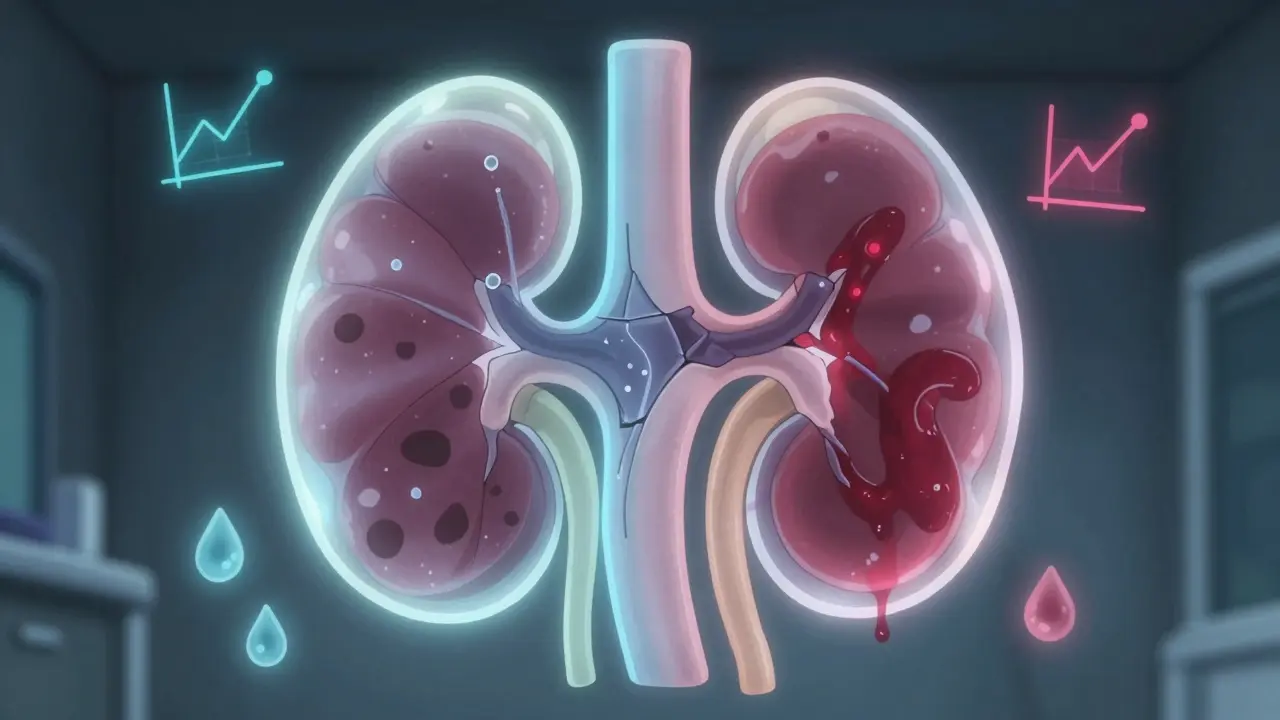
Your kidneys filter about 120-150 quarts of blood every day. They remove waste, balance fluids, regulate electrolytes, and help control blood pressure. When AKI hits, that filter slows or stops. It’s not a full shutdown like in movies-you might still pee, but your body starts drowning in its own toxins.
The medical definition is simple: a rise in serum creatinine by 0.3 mg/dL in 48 hours, or a 50% jump from your normal level within a week. Or, if you’re making less than half a milliliter of urine per kilogram of body weight for six hours straight. These aren’t arbitrary numbers. They’re red flags that your kidneys are in trouble.
Here’s the catch: about 22% of people with AKI don’t feel a thing. No swelling. No pain. No nausea. Just a routine blood test that says, ‘Something’s wrong.’ That’s why hospitals now monitor creatinine every 24 to 48 hours for high-risk patients-like those in the ICU, older adults, or people with diabetes or heart failure.
Three Main Causes-And Why It Matters
Not all AKI is the same. Where it starts changes everything.
Prerenal (60-70% of cases) means your kidneys aren’t getting enough blood. This isn’t damage to the organ itself-it’s a supply problem. Causes? Dehydration from vomiting or diarrhea, heavy bleeding, heart failure, or even just being on too many blood pressure meds. The kidneys are fine. They’re just starving. Give them fluid, and they often bounce back in 24 to 48 hours.
Intrarenal (25-35%) is the real damage. Something is hurting the kidney tissue. The most common culprit? Acute tubular necrosis (ATN), where the tiny tubes inside the kidney die off. This often comes after a severe infection, major surgery, or exposure to toxins. Common offenders? Antibiotics like gentamicin, contrast dye used in CT scans, or even too much ibuprofen. This kind of AKI takes longer to heal-weeks, sometimes months.
Postrenal (5-10%) is a blockage. Think of it like a clogged sink. If your ureters or bladder get blocked-by an enlarged prostate, kidney stones, or a tumor-urine backs up and crushes the kidney from the inside. This one is often fixable fast. Insert a stent, remove the stone, and kidney function can improve within hours.
What Symptoms Should You Watch For?
Symptoms vary wildly. Some people feel terrible. Others feel fine.
- Urine output drops below 400 mL a day (oliguria) or stops entirely (anuria)
- Swelling in legs, ankles, or face from fluid buildup
- Shortness of breath from fluid in the lungs
- Extreme fatigue, dizziness, or confusion
- Nausea, vomiting, or loss of appetite
- Flank pain (back pain just below the ribs)
- Chest pain from inflammation around the heart (pericarditis)
But here’s what most people don’t realize: you can have all of these and still not know it’s your kidneys. That’s why lab tests are non-negotiable in high-risk situations.
How Doctors Diagnose It
It starts with blood and urine tests.
Serum creatinine is the gold standard. But it’s slow. It can take 24 to 48 hours to rise after kidney damage starts. That’s why newer tools are emerging. Tests for biomarkers like NGAL (neutrophil gelatinase-associated lipocalin) can flag AKI 24 to 48 hours before creatinine changes. Some hospitals are already using them.
BUN (blood urea nitrogen) often rises too, but it’s less specific-it can go up with dehydration or high protein intake.
Urine output is tracked hourly in the ICU. A drop below 0.5 mL/kg/hour for six hours is a diagnostic trigger.
Ultrasound is used in 85% of cases to check for blockages or kidney size. A shrunken, echo-bright kidney suggests chronic damage. A normal-sized kidney with obstruction? That’s fixable.
FeNa (fractional excretion of sodium) helps tell the difference between prerenal and intrarenal causes. Below 1%? Likely dehydration. Above 2%? Likely kidney damage.
How It’s Treated-It Depends on the Cause
Treatment isn’t one-size-fits-all. It’s targeted.
Prerenal AKI: Fluids. Simple. Fast. A 500-1000 mL IV saline bolus often turns things around. No dialysis needed. Most recover fully.
Intrarenal AKI: Stop the toxin. If it’s an antibiotic, stop it. If it’s contrast dye, avoid it next time. For glomerulonephritis, steroids or immunosuppressants might be needed. In severe ATN, dialysis may be required until the kidney heals. Recovery can take 2 to 6 weeks.
Postrenal AKI: Remove the blockage. A stent in the ureter? Done in minutes. A catheter for an enlarged prostate? Often life-saving. Once the pressure is off, kidneys can recover quickly-even if they’ve been under strain for days.
When things get critical-high potassium, fluid overload, or acid buildup-renal replacement therapy kicks in. Hemodialysis is common in hospitals. CRRT (continuous renal replacement therapy) is used in ICU patients who are unstable. Peritoneal dialysis? Rare, but used when veins are hard to access.
Recovery: What to Expect
Recovery isn’t guaranteed. It depends on how bad it was, how long it lasted, and your baseline health.
- Prerenal AKI: 70-80% recover fully within a week
- Intrarenal AKI: 40-60% recover partially or fully over weeks
- Severe ATN with long oliguria (>14 days): Only 20-30% fully recover
Age matters. If you’re over 65, your recovery rate drops by 35%. If you already had reduced kidney function before (eGFR under 60), your chance of full recovery drops by half.
And if you needed dialysis? Only 25% get back to full kidney function within three months.
But here’s the hopeful part: many people do recover. A patient in Halifax had AKI from dehydration after a stomach bug. Creatinine jumped from 0.9 to 1.8. Two liters of IV fluids in the ER. Back to normal in 24 hours. No lasting damage.
The Hidden Aftermath: What No One Tells You
Even after your creatinine returns to normal, your body isn’t done.
A 2022 survey of over 1,200 AKI survivors found that 68% felt exhausted for 3 to 6 months. Not just tired-bone-deep fatigue. 42% had ongoing anxiety about their kidneys. 29% couldn’t return to work because they couldn’t walk more than 50 feet without gasping.
And here’s the big one: 23% of AKI survivors develop chronic kidney disease within a year. Each episode of AKI raises your 5-year risk of needing dialysis by over 8 times.
That’s why follow-up is critical. If you’ve had AKI, you need to see a nephrologist within 6 months. Get your eGFR checked. Monitor your blood pressure. Avoid NSAIDs. Stay hydrated. These aren’t suggestions-they’re survival steps.
What’s Changing Now
The field is moving fast.
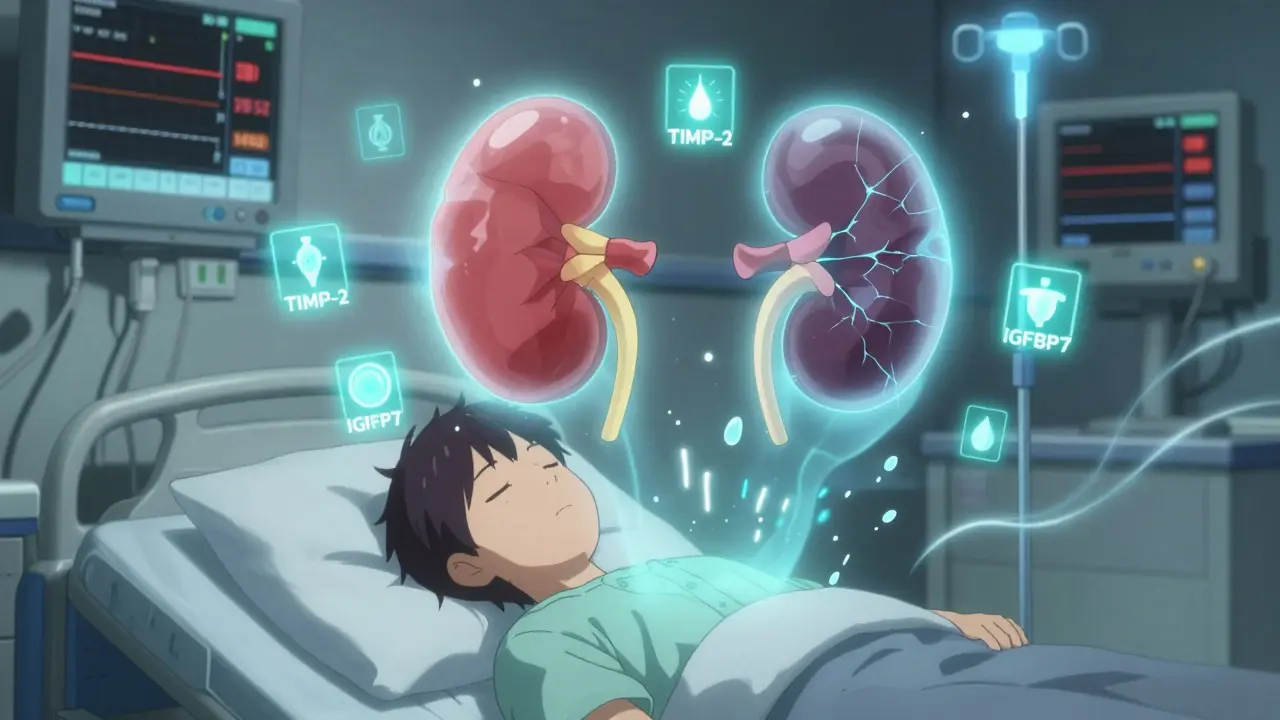
Researchers are testing new biomarkers like TIMP-2 and IGFBP7 that can predict AKI 12 hours before it shows up on labs. AI tools are being trained to scan electronic health records and flag patients at risk-up to 24 hours before symptoms start.
The STARRT-AKI trial showed that starting dialysis earlier in severe cases cut 90-day death rates by 9%. That’s huge.
And in 2021, NICE updated guidelines to recommend point-of-care testing for NGAL in high-risk patients. That’s already happening in major Canadian hospitals.
These aren’t futuristic ideas. They’re in use now.
What You Can Do
If you’re at risk-older, diabetic, on blood pressure meds, or recently hospitalized-know the signs. Ask for your creatinine level after any illness or procedure. Don’t assume ‘normal’ means fine.
Hydrate. Avoid NSAIDs like ibuprofen unless your doctor says it’s safe. Tell every new doctor you’ve had AKI before. It changes how they treat you.
Recovery isn’t just about labs going back to normal. It’s about protecting what’s left. One episode of AKI changes your kidney’s future. Treat it like the emergency it is-because it is.
13 Comments
AKI isn’t some minor glitch-it’s a full-system alert. If you’re over 60, on meds, or had recent surgery, stop ignoring your labs. Your kidneys don’t scream. They whisper. And by the time you hear it, it’s too late.
Prerenal AKI is still the most common and most treatable-if caught early. The key is FeNa and urine output trends, not just creatinine. NGAL is game-changing in ICUs. Hospitals that still rely on creatinine alone are operating in the 90s.
my aunt had this after a bad flu and they gave her iv fluids and she was fine in a day but now shes scared to even take tylenol and its kinda sad because she cant even enjoy a beer on the weekend anymore
I’ve seen this play out in my dad’s ICU unit-patients who didn’t even know something was wrong until their numbers spiked. But here’s the thing: recovery isn’t just about numbers. It’s about the quiet exhaustion that sticks around for months. The fatigue that makes you feel like you’re wading through molasses just to get out of bed. That’s the hidden cost. And no one talks about it. We fix the labs but forget the person.
My dad’s nurse told me once: ‘We bring the creatinine down. But we don’t always bring the soul back up.’
It is both scientifically and ethically indefensible that healthcare institutions continue to rely upon serum creatinine as the primary biomarker for acute kidney injury, given its well-documented lag time of 24 to 48 hours. The literature has unequivocally demonstrated the superior sensitivity and specificity of NGAL, TIMP-2, and IGFBP7 for early detection. The continued non-adoption of these validated biomarkers constitutes a systemic failure in clinical diligence, particularly within non-academic settings. Furthermore, the failure to mandate nephrology follow-up within six months post-AKI-despite the 23% progression rate to chronic kidney disease-is not merely negligent; it is a dereliction of professional duty.
…and yet, despite all this ‘evidence,’ no one mentions that the real driver of AKI isn’t ibuprofen or dehydration-it’s the pharmaceutical-industrial complex pushing NSAIDs as ‘safe’ while quietly funding studies that downplay renal risk. The fact that NICE only ‘recommended’ NGAL testing in 2021? That’s not progress. That’s damage control. And don’t get me started on CRRT-costly, invasive, and overused because hospitals don’t want to admit they missed the early signs.
so like… is this why they wont let me get a ct scan without a blood test? i thought they were just being annoying but now im like… ohhhhhh
you know what they dont tell you? the government is using AKI stats to push people into dialysis so they can sell more machines to hospitals. they even made up the ‘chronic kidney disease’ label to keep you scared and buying meds. i know a guy who got dialysis for 3 months and then just drank lemon water and his kidneys came back to normal. they dont want you to know that.
👍💊🩺💧
This is such a clear breakdown. I’m from India, and here, people often think ‘no pain = no problem.’ But AKI doesn’t care. My cousin had it after a fever and antibiotics-he thought he was fine until he collapsed. Now he’s on monthly checkups. Awareness saves lives.
Good post. My uncle had prerenal AKI after a long trip with no water. They gave him fluids and he was back in two days. Just drink water. Don’t wait until you’re dizzy.
why do i have to care about my kidneys? they’re just organs. i’m not gonna stress over a blood test. i’ve got other stuff to worry about.
While the clinical framework presented is accurate and well-structured, it is imperative to acknowledge the socioeconomic disparities that limit access to biomarker testing and nephrology follow-up. The assumption that all patients can receive NGAL assays or timely specialist referrals is a privilege, not a standard. In rural and underserved communities, even basic creatinine monitoring remains inconsistent. Without systemic intervention, these protocols remain theoretical for the majority.
Thanks for this. I’m a nurse and I’ve seen too many patients dismissed because ‘they look fine.’ Your point about follow-up is spot on. If you’ve had AKI, you’re not ‘cured.’ You’re on watch. Tell every doctor. Write it on your chart. Don’t let them forget it.
Write a comment