Calcium Channel Blocker Interaction Checker
Your Calcium Channel Blocker
Additional Medications/Supplements
Health Factors
Calcium channel blockers (CCBs) are among the most commonly prescribed heart medications in the U.S., with over 50 million people using them to treat high blood pressure, chest pain, or irregular heartbeats. But for many, the real danger isn’t the drug itself-it’s what it does when mixed with other pills, foods, or even natural supplements. The problem isn’t just about side effects. It’s about how your body breaks down these drugs, and what happens when that process gets disrupted.
How Calcium Channel Blockers Work-and Why They’re So Sensitive
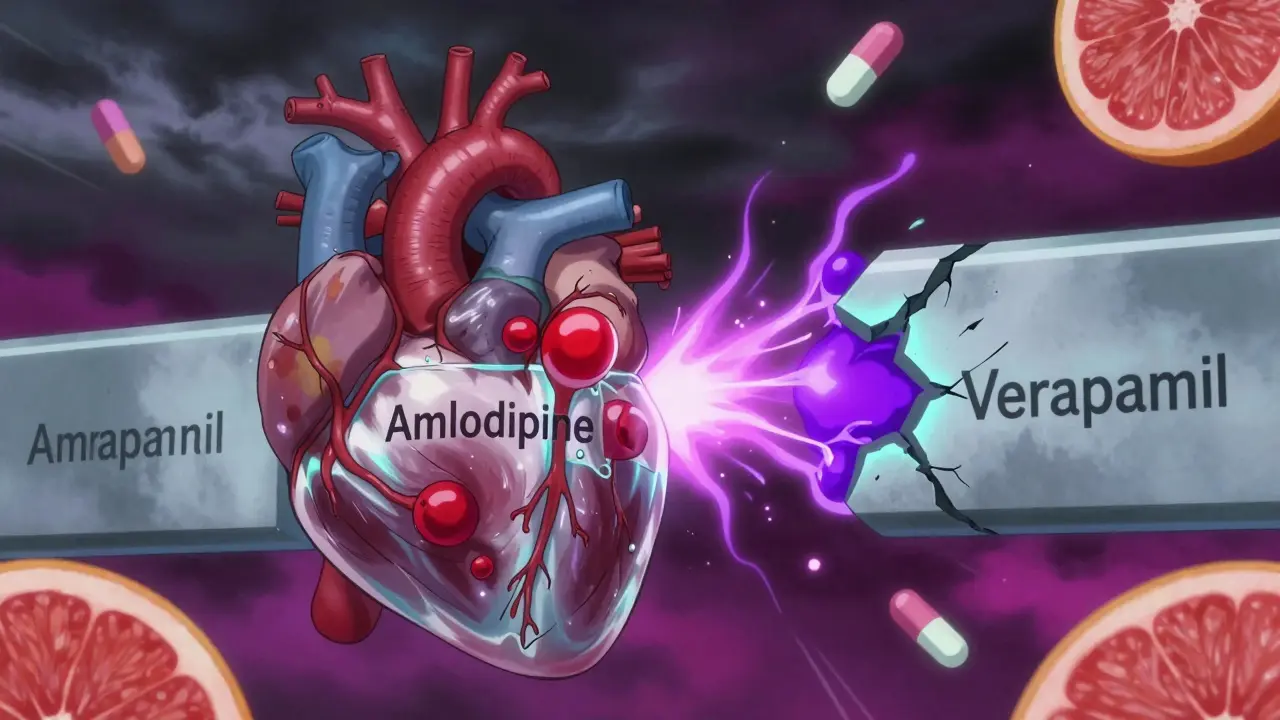
Calcium channel blockers stop calcium from entering heart and blood vessel cells. This relaxes your arteries, lowers blood pressure, and slows heart rate. But not all CCBs are the same. They’re split into two groups: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine; and non-dihydropyridines like verapamil and diltiazem.
DHPs mainly affect blood vessels. That’s why amlodipine is the most prescribed-it’s good at lowering blood pressure without slowing the heart too much. Non-DHPs like verapamil and diltiazem hit both the heart and blood vessels. That makes them useful for arrhythmias, but also riskier when combined with other drugs.
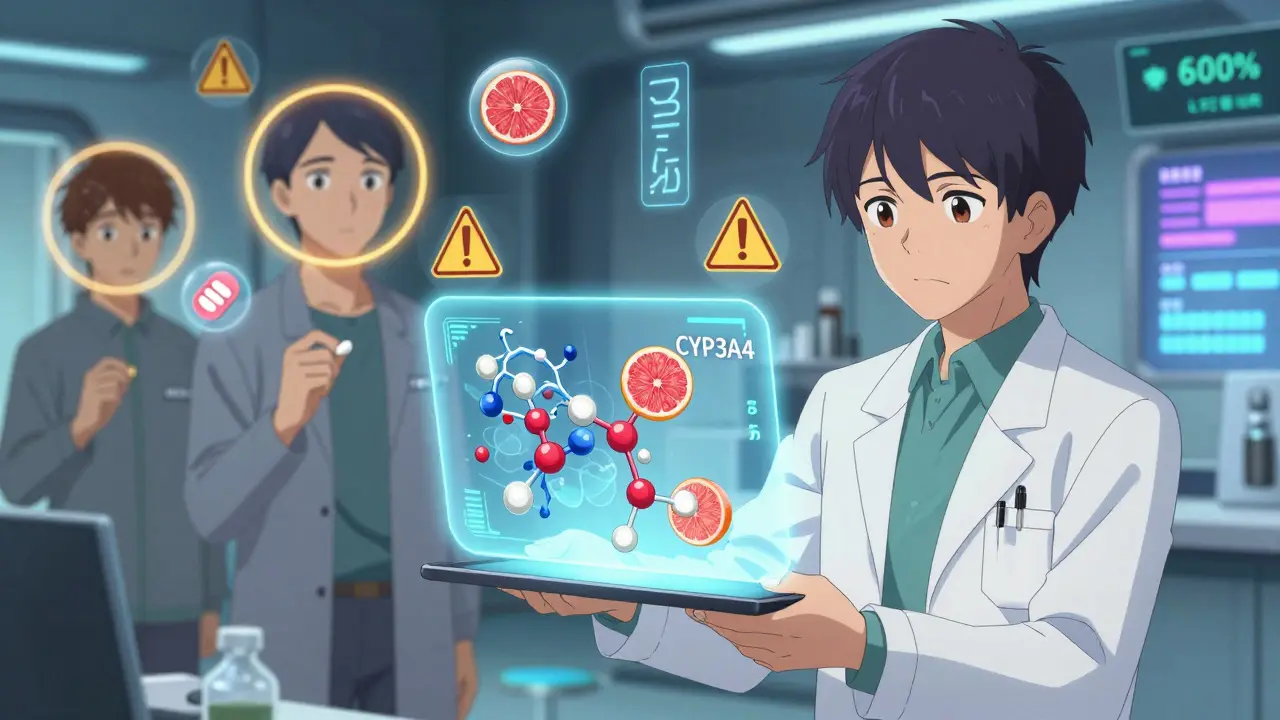
Here’s the catch: almost all CCBs are broken down by one enzyme-CYP3A4. This enzyme lives mostly in your liver and gut. It’s responsible for processing about half of all prescription drugs. When CYP3A4 is working normally, CCBs get broken down and cleared safely. But if something blocks or slows CYP3A4, the drug builds up in your blood. Too much can mean dangerously low blood pressure, slow heart rate, or even heart block.
The Biggest Culprits: What Slows Down Drug Clearance
Some of the most common things people take can dramatically increase CCB levels. Grapefruit juice is the classic example. Just one glass can reduce CYP3A4 activity by up to 60% for 24 hours. For someone on nifedipine or felodipine, that’s enough to cause dizziness, fainting, or a trip to the ER. Over 68% of patients who reported problems on Mayo Clinic’s forum linked their low blood pressure to grapefruit juice.
Antibiotics like clarithromycin and antifungals like ketoconazole are even worse. These are strong CYP3A4 inhibitors. When taken with verapamil, they can spike drug levels by 300-600%. The European Society of Cardiology has documented 17 cases where this combo caused complete heart block-requiring a pacemaker.
Even some HIV meds like ritonavir and the antidepressant fluoxetine interfere. And don’t forget diltiazem itself. It doesn’t just get broken down by CYP3A4-it also blocks it. That’s why combining diltiazem with statins like simvastatin can cause muscle damage. One study showed simvastatin levels jumping 400%.
Verapamil is especially dangerous because it also blocks a transporter called P-glycoprotein. This means it doesn’t just affect metabolism-it also stops your body from flushing out other drugs like digoxin. When digoxin builds up, it can cause deadly heart rhythms. Patients on both drugs need frequent blood tests to check digoxin levels.
Amlodipine: The Safer Choice for Complex Medication Regimens
If you’re taking five or more medications, amlodipine is usually the best CCB option. Why? Because it barely inhibits CYP3A4. It’s a substrate-meaning it gets broken down by the enzyme-but it doesn’t interfere with it. That makes it far less likely to cause interactions.
Studies show that only 12% of patients on amlodipine need a dose change when taking moderate CYP3A4 inhibitors. Compare that to diltiazem, where 45% require adjustments. Amlodipine also has a long half-life-30 to 50 hours-so it’s taken once daily and doesn’t cause wild spikes in blood levels.
Its protein binding is high (97.5%), but that doesn’t lead to major interactions because it doesn’t compete with other drugs for binding sites. And unlike verapamil, it doesn’t affect digoxin or other P-glycoprotein substrates. That’s why cardiologists now recommend amlodipine as first-line for older adults on multiple meds.
Age, Kidney Function, and Genetic Risk: Hidden Factors
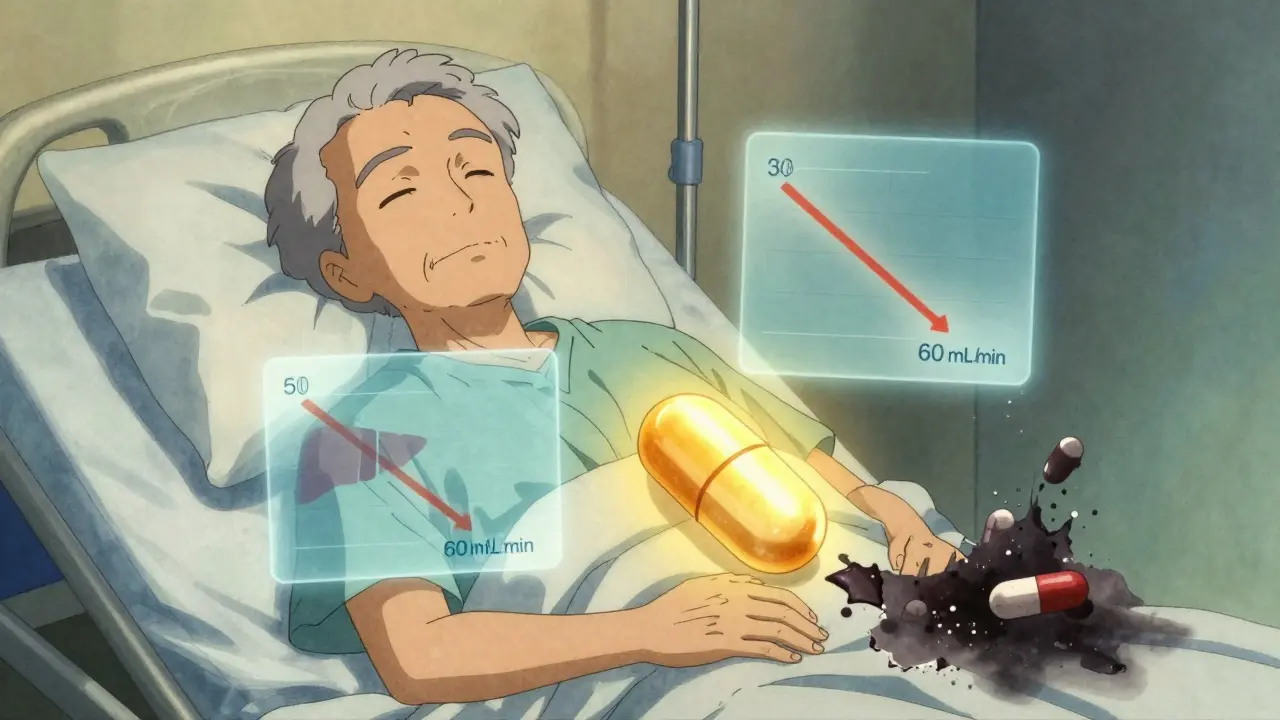
Metabolic interactions aren’t the same for everyone. Older adults are at higher risk-not just because they take more drugs, but because their liver and kidney function decline. By age 65, CYP3A4 activity drops by 30-40%. Add in reduced kidney clearance, and even normal doses can become toxic.
Patients with an eGFR below 60 mL/min (moderate kidney disease) face a 47% higher risk of severe interactions. Verapamil requires a 50% dose reduction in these patients. Amlodipine? No adjustment needed. That’s a key difference many doctors overlook.
Genetics play a role too. About 27% of people have genetic variants that make CYP3A4 work slower or faster. If you’re a slow metabolizer, even standard doses of verapamil can build up. A new $15 million NIH study is tracking these variants to create personalized dosing rules. By 2027, genetic testing may be standard before prescribing CCBs.
Real-World Problems: What Patients Are Reporting
Online forums and patient reviews paint a grim picture. On Drugs.com, CCBs have a 3.2/5 rating for side effects-lower than their 4.1/5 for effectiveness. The top complaint? Unexpected low blood pressure.
One Reddit user described passing out after taking amlodipine with a common antifungal cream. Another reported chest pain after combining verapamil with a herbal supplement. A 72-year-old woman on diltiazem and simvastatin developed muscle weakness so severe she couldn’t climb stairs. All three cases were avoidable with proper interaction screening.
On Healthgrades, 73% of negative reviews mention interaction-related side effects. And 42% of those involve combining CCBs with erectile dysfunction drugs like sildenafil. Verapamil users are nearly four times more likely to have dangerous drops in blood pressure than those on amlodipine.
What Doctors and Pharmacies Are Doing About It
Hospitals and clinics are finally catching up. The Cleveland Clinic now requires all new CCB prescriptions to be screened for CYP3A4 interactions. They found 23% of patients were at high risk. For those patients, they start with amlodipine at 2.5 mg instead of 5 mg-and 78% stick with the plan.
Community pharmacists spend nearly 13 minutes per CCB prescription checking for interactions. They catch 18% of risky combinations before the patient leaves the pharmacy. EHR systems like Epic now flag high-risk combos automatically. Since 2022, severe interaction events have dropped 42% in clinics using these alerts.
There’s even a new FDA-approved tool called CCB-Check, integrated into electronic records. It gives real-time risk scores and has cut hospitalizations from CCB interactions by 31% in just six months.
What You Should Do
If you’re on a calcium channel blocker:
- Never drink grapefruit juice without checking with your doctor.
- Always list every medication, supplement, and herb you take-even over-the-counter ones.
- Ask if your CCB is amlodipine. If not, ask if switching would be safer.
- If you’re over 65 or have kidney problems, make sure your dose is adjusted.
- Watch for dizziness, fainting, slow pulse, or swelling in your legs-these could be signs of buildup.
- Get your blood pressure checked within 2 hours of starting a new drug or changing a dose.
Most importantly: don’t assume your doctor knows every drug you’re taking. Bring a full list to every appointment. If your pharmacist flags an interaction, don’t brush it off. These aren’t theoretical risks-they’re life-threatening.
What’s Next for Calcium Channel Blockers
The global CCB market is worth over $5 billion. But prescriptions for verapamil and diltiazem are falling. Amlodipine now makes up 42% of all CCB sales. Why? Because it’s safer in the real world-where people take multiple drugs, eat grapefruit, and get older.
By 2027, personalized dosing based on genetics, liver function, and drug history will likely become standard. Until then, the best protection is awareness. Know your meds. Know your risks. And never ignore a warning about interactions.
Can I drink grapefruit juice while taking calcium channel blockers?
No, you should avoid grapefruit juice entirely if you’re taking nifedipine, felodipine, or verapamil. Even a single glass can block the enzyme (CYP3A4) that breaks down these drugs, causing dangerous spikes in blood levels. This can lead to severe low blood pressure, dizziness, or fainting. Amlodipine is less affected, but it’s still safer to avoid grapefruit juice altogether unless your doctor confirms it’s okay.
Which calcium channel blocker has the fewest drug interactions?
Amlodipine has the fewest drug interactions among calcium channel blockers. Unlike verapamil and diltiazem, it doesn’t significantly inhibit CYP3A4 or P-glycoprotein. It’s also not affected much by moderate inhibitors, and its long half-life means stable blood levels. For patients on multiple medications, especially older adults, amlodipine is the preferred choice for safety.
Why does verapamil interact more than amlodipine?
Verapamil is both a substrate and a strong inhibitor of CYP3A4, meaning it slows down its own metabolism and the metabolism of other drugs. It also blocks P-glycoprotein, which increases levels of drugs like digoxin. Amlodipine is only a substrate-it doesn’t inhibit enzymes or transporters. This dual role makes verapamil far more likely to cause dangerous interactions, especially with antibiotics, antifungals, or statins.
Can kidney problems make calcium channel blocker interactions worse?
Yes. While most CCBs are cleared by the liver, their metabolites are removed by the kidneys. If your kidney function is low (eGFR below 60), these metabolites can build up and increase side effects. Verapamil requires a 50% dose reduction in moderate kidney disease. Amlodipine doesn’t need adjustment because its metabolites are less active. Always check your eGFR before starting or changing a CCB.
Are there tests to check if I’m at risk for CCB interactions?
Yes. Therapeutic drug monitoring can measure blood levels of verapamil and diltiazem to ensure they’re in the safe range (50-150 ng/mL). Genetic testing for CYP3A4 variants is also available and can identify if you’re a slow metabolizer. While not routine yet, these tests are becoming more common, especially for patients on multiple drugs or with unexplained side effects. Ask your doctor if testing is right for you.
If you’re on a calcium channel blocker and taking other medications, don’t guess. Talk to your pharmacist or doctor. A simple check can prevent an emergency.
14 Comments
Ugh I just found out my grandma was taking amlodipine with grapefruit juice and didn’t even know it was dangerous. She passed out last week. Thank you for this post. I’m going to print this out and tape it to her fridge. 🙏
Look, I get it, amlodipine is the ‘safe’ CCB, but let’s not pretend the pharmaceutical industry isn’t pushing it because it’s patent-protected and profitable. Verapamil’s been around since the 70s, cheap as dirt, and works great for arrhythmias. The real issue? Doctors don’t have time to explain interactions, so they just prescribe the ‘easiest’ drug. Meanwhile, the grapefruit juice myth gets amplified while real polypharmacy chaos goes ignored. Also, why are we still using CYP3A4 as the sole metric? What about gut microbiome variations? Nobody talks about that. #BigPharmaIsWatching
It is imperative to note, however, that the metabolic pathways described herein are not universally applicable across all patient populations-particularly those with hepatic comorbidities, or those who are CYP3A4*22 carriers, which, according to PharmGKB, reduces enzyme activity by approximately 20-30%. Furthermore, the assertion that amlodipine is ‘safe’ in polypharmacy contexts is misleading; while it does not inhibit CYP3A4, it is still subject to competitive displacement by highly protein-bound agents such as warfarin and phenytoin. Additionally, the claim regarding the 97.5% protein binding is irrelevant without context: binding displacement is not the primary concern-metabolic inhibition is. Therefore, I must respectfully correct the narrative.
My dad was on diltiazem and simvastatin for years. Never knew why he was so tired until his pharmacist flagged it. Switched to amlodipine and he’s been hiking again. Simple fix. Don’t overcomplicate it.
They’re not drugs. They’re landmines. And we’re all walking through a minefield wearing blindfolds.
So… what you’re saying is, if you’re old, poor, and on meds, you’re just supposed to trust the system? Funny how the same system that pushes these drugs also makes it impossible to get genetic testing unless you’re rich. Maybe the real problem isn’t grapefruit juice-it’s that we treat people like data points with kidneys.
Thank you for writing this. I’ve been telling my mom for years not to drink grapefruit juice with her meds, but she thinks it’s ‘natural’ so it’s fine. Now I’m sending her this. Also, amlodipine FTW. I’m on it and I feel like a normal human again. 😊
America’s healthcare is broken. We need to ban grapefruit juice and force doctors to test everyone’s liver before prescribing. This is why we can’t have nice things.
This is so important… I had no idea diltiazem could affect digoxin like that… My aunt had that exact issue last year… I’m going to share this with my whole family… 💔 I just wish more people knew…
Of course the system ignores this. Big Pharma doesn’t want you to know that your $100-a-month drug could kill you if you eat a damn grapefruit. They’d rather you die quietly than admit they didn’t test for real-world chaos. And now they’re selling you ‘CCB-Check’ like it’s a magic wand. It’s not a tool-it’s a liability shield.
They're hiding the truth. CYP3A4 isn't the problem. The real issue is the government's secret biochip program that tracks your meds through your toilet. Grapefruit juice? A distraction. They want you to panic over fruit so you don't ask why your insulin dose changed after you got the flu shot.
While the post correctly identifies CYP3A4-mediated interactions, it fails to contextualize the pharmacokinetic-pharmacodynamic (PK-PD) disconnect in elderly populations. The absence of QT interval monitoring recommendations is a critical omission. Furthermore, the assertion that amlodipine is ‘safer’ lacks statistical power in the cited studies-most were retrospective cohort analyses with confounding by indication. This is anecdotal medicine dressed as evidence.
My brother died from a CCB interaction. They told him grapefruit juice was fine. He was 47. This isn’t science. This is negligence. And you’re all just commenting like it’s a TikTok trend.
Okay but… why are we still talking about CCBs like they’re the only dangerous drugs? What about statins? NSAIDs? SSRIs? We’re just picking on calcium blockers because they’re old and boring? This feels like a witch hunt with a PubMed citation.
Write a comment