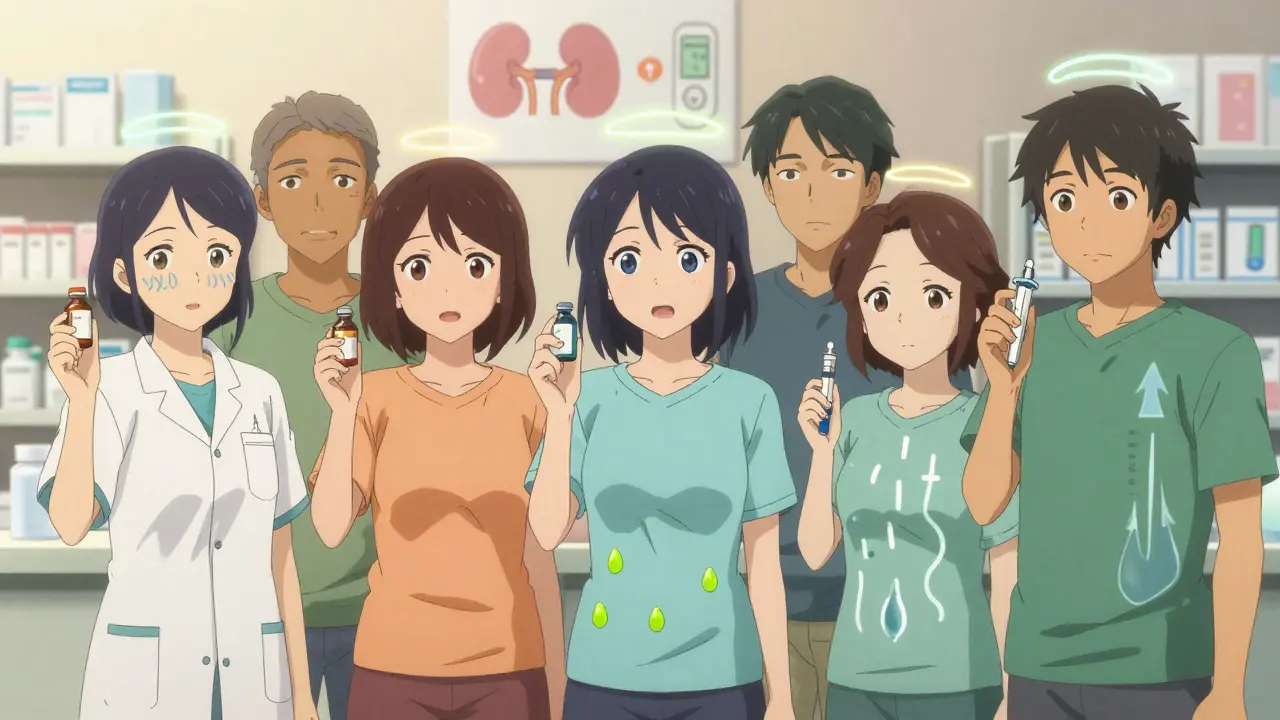
When you're managing diabetes, the goal is simple: keep your blood sugar steady so you don't end up in the hospital or lose a toe to nerve damage. But the pills and injections that help you get there? They come with their own set of surprises. Some people feel fine on metformin. Others can't even keep toast down. One person loses 12 pounds on a GLP-1 drug. Another ends up in the ER with a yeast infection they didn't see coming. If you're new to diabetes meds or stuck on one that's making life harder, here's what you actually need to know - no fluff, just what works, what hurts, and what to do next.
Metformin: The First Line, But Not for Everyone
Metformin is still the go-to starter for type 2 diabetes. It’s cheap, it’s been around for decades, and it doesn’t make you gain weight. In fact, it might even help you lose a little. But if you’ve ever thrown up after taking it on an empty stomach, you’re not alone. About 1 in 3 people get stomach upset - nausea, cramps, diarrhea. It usually fades after a few weeks, but for some, it doesn’t. A 2021 study in JAMA Internal Medicine found 26% of users had nausea, 23% had diarrhea. That’s why doctors now start low: 500 mg once a day with dinner. Some switch to the extended-release version, which cuts GI side effects by half. Long-term users should get their vitamin B12 checked yearly. Metformin can drain it over time. Low B12 means fatigue, tingling hands, even memory issues. Fixing it? A monthly B12 shot or high-dose pill. Easy fix. Hard to know unless you ask.
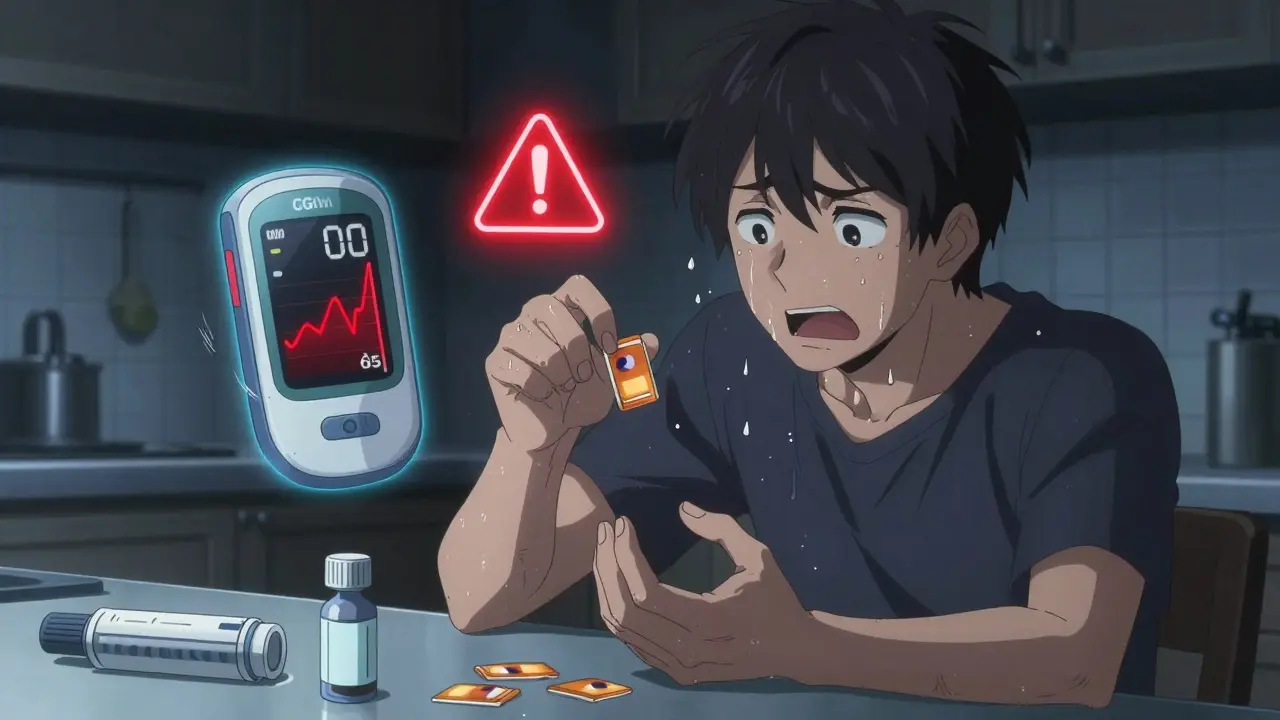
Sulfonylureas: Low Blood Sugar Lurks
Drugs like glyburide and glipizide work by forcing your pancreas to pump out more insulin. Sounds good - until your blood sugar drops too far. Hypoglycemia is the big risk here. About 1 in 6 users have at least one scary low-blood-sugar episode every year. Symptoms? Sweating, shaking, confusion, passing out. Some people get so scared they skip doses. A 2020 study found skipping meals triples your chance of going low. And yes, you’ll probably gain 2 to 4 kilos. These drugs are still used, especially where cost matters. But if you’re active, eat irregularly, or live alone? They’re risky. Many patients switch to newer options just to avoid the fear.
Thiazolidinediones: Weight Gain and Heart Risks
Pioglitazone (Actos) makes your body use insulin better. It works. But it also makes you hold water. About 1 in 20 users get swelling in their legs. That’s a red flag for heart failure - especially if you already have heart issues. A 2005 study in The Lancet showed a 43% higher chance of heart failure with these drugs. They also cause weight gain, mostly from fat and fluid. Most doctors won’t touch them unless other options fail. And rosiglitazone (Avandia)? It got pulled in 2011 over heart risks. Even though it came back with restrictions, few prescribers use it anymore. These aren’t first choices anymore. They’re last-resort.
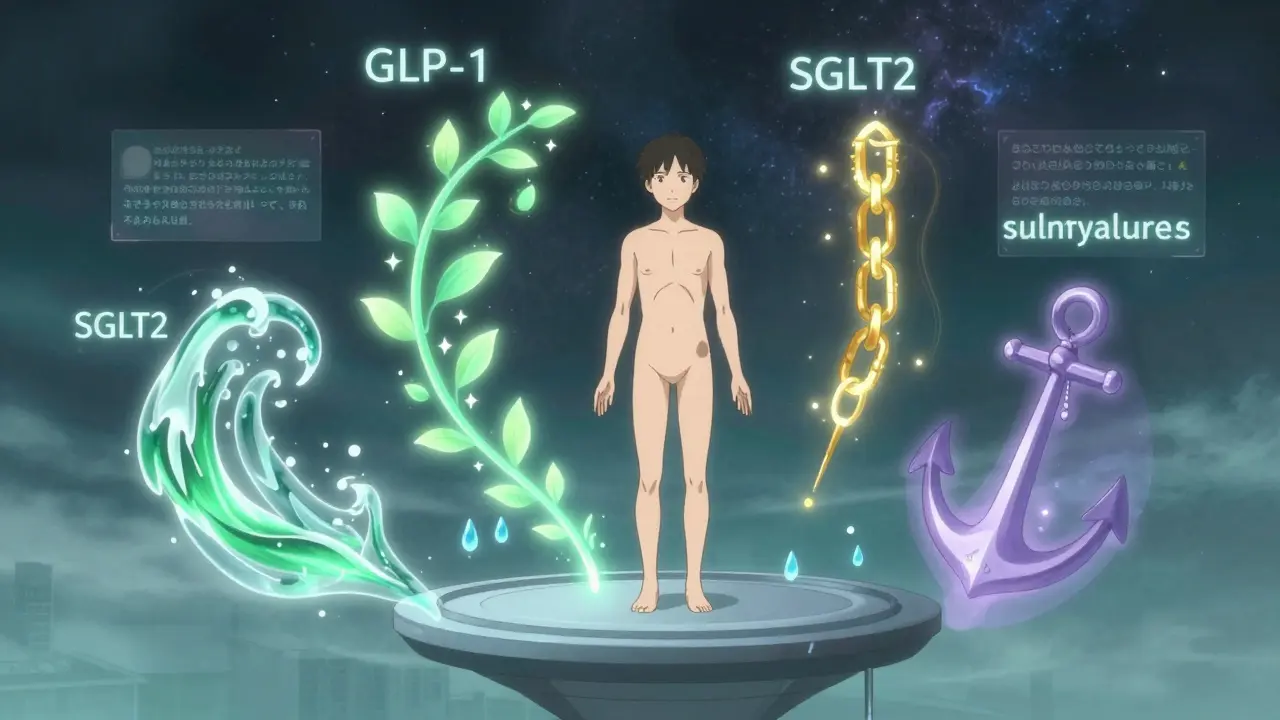
SGLT2 Inhibitors: The New Kids on the Block
Dapagliflozin (Farxiga), empagliflozin (Jardiance), and canagliflozin (Invokana) work differently. They tell your kidneys to pee out extra sugar. That lowers blood sugar - and helps you lose weight. But there’s a catch. You’re peeing out glucose, which means your genital area gets wetter and sweeter. For women, that’s yeast infections. About 1 in 7 get them. For men? It’s 1 in 20. Some say it’s just annoying. Others say it ruins their sex life. A Reddit survey in late 2023 found 73% of users had this issue. The fix? Wear cotton underwear, dry well after showers, skip douches. Also, these drugs can cause dehydration. If you’re sick, skip them. You could get dangerously low on fluids. And yes - ketoacidosis. Rare, but real. Less than 1 in 500, but it can hit hard. If you’re vomiting, feeling sick, and have fruity-smelling breath? Go to the ER. These drugs also cut heart and kidney risks. That’s why doctors now push them for people with heart disease or kidney problems. The EMPA-KIDNEY trial in 2023 proved they protect kidneys even if you don’t have diabetes.
GLP-1 Receptor Agonists: Weight Loss and Stomach Chaos
Liraglutide (Victoza), semaglutide (Ozempic, Wegovy), and exenatide (Byetta) mimic a gut hormone that slows digestion and tells your pancreas to make insulin - only when needed. They’re powerful. In studies, people lost 5 to 10 pounds on average. Some lost more. But nausea? It’s common. Up to half of users feel sick. Vomiting? 1 in 5. Diarrhea? 1 in 3. It usually gets better after 4 to 6 weeks. If it doesn’t? Talk to your doctor. Dose ramp-up matters. Start low. Move slow. These drugs also cut heart attack and stroke risk by up to 26% in high-risk patients. That’s why they’re now recommended for people with heart disease or obesity. The new one, tirzepatide (Mounjaro), combines two hormones and causes less nausea. Weight loss? Up to 20% of body weight in trials. But they cost $800 to $900 a month without insurance. And they’re injections. Not pills.
Insulin: The Most Effective - and Riskiest
Insulin is the only option for type 1 diabetes. Many with type 2 end up on it too. It works. But it demands precision. Too much? You crash. Too little? You burn. The DCCT trial from 1993 showed people on intensive insulin had 15 to 30 low-blood-sugar episodes per year. That’s more than one a week. Fear of lows makes people under-dose. A 2022 survey found 1 in 3 insulin users intentionally skip doses to avoid hypoglycemia. That’s dangerous. The 15-15 rule helps: 15 grams of sugar (juice, glucose tabs), wait 15 minutes, check again. Continuous glucose monitors (CGMs) cut severe lows by 40%. New long-acting insulins like insulin glargine (Lantus) and insulin degludec (Tresiba) are steadier. Less bumpiness. Less risk. But you still gain weight - 2 to 5 kilos. And injections? Not everyone likes them. But for many, they’re the only thing that keeps their sugar in check.
What to Do If Side Effects Hit
Don’t quit cold turkey. Talk to your doctor. For metformin? Switch to extended-release. For nausea from GLP-1 drugs? Slow the dose increase. For yeast infections from SGLT2 inhibitors? Change your underwear. For hypoglycemia? Get a CGM. Keep fast-acting carbs in your bag. Test your blood sugar before driving. If you’re scared of lows, ask about a glucagon kit. Your doctor can prescribe one. And if cost is a problem? Generic metformin costs $4 a month. Insulin? Some brands are now $35 a vial in the U.S. Ask about patient assistance programs. The American Diabetes Association has a list. You’re not alone. Most people on these meds have struggled with side effects. The trick isn’t avoiding them - it’s managing them before they manage you.
What’s Changing in 2026?
New drugs keep coming. In 2023, the FDA approved orforglipron, an oral GLP-1 pill. No needles. Just a capsule. Early results show weight loss similar to injections. And basal insulin icodec, a once-weekly insulin shot, is now approved in Europe. Coming to the U.S. soon. These aren’t just fancy upgrades. They’re about making life easier. But access is still unequal. One in four U.S. patients skip doses because of cost. Black and Latino patients are less likely to get newer drugs, even when they’d benefit most. The system isn’t fair. But knowledge is power. Know your options. Ask for help. Your health matters more than the price tag.
Can I stop my diabetes medication if I feel better?
No. Feeling better doesn’t mean your diabetes is gone. Medications manage blood sugar, but they don’t cure the condition. Stopping without medical advice can cause your sugar to spike quickly, leading to nerve damage, kidney strain, or even diabetic ketoacidosis. Even if you’ve lost weight or changed your diet, always talk to your doctor before adjusting or stopping any drug.
Why do some diabetes pills cause weight gain while others cause weight loss?
It depends on how the drug works. Medications like sulfonylureas and insulin push your body to store more glucose as fat, leading to weight gain. GLP-1 agonists and SGLT2 inhibitors do the opposite. GLP-1 drugs slow digestion and reduce appetite. SGLT2 drugs make you pee out sugar - and with it, calories. That’s why you lose weight. It’s not magic. It’s science. And it’s why newer drugs are preferred for people who need to lose weight or have heart disease.
Is metformin safe long-term?
Yes, for most people. Metformin has been used safely for over 60 years. The main long-term risk is vitamin B12 deficiency, which affects 10% to 30% of users after five years. It’s easily checked with a blood test and fixed with supplements. Kidney function matters too - if your eGFR drops below 30, your doctor will stop it. Otherwise, it’s one of the safest, most effective drugs for type 2 diabetes.
Which diabetes medication has the fewest side effects?
Metformin has the fewest serious side effects for most people. It doesn’t cause low blood sugar on its own and doesn’t lead to weight gain. The biggest issue is stomach upset, which often fades with time or by switching to extended-release. For people with heart or kidney disease, SGLT2 inhibitors or GLP-1 agonists may be safer overall because they reduce complications - even if they cause more minor side effects.
Can I take diabetes meds if I’m pregnant?
Most oral diabetes drugs are not recommended during pregnancy. Metformin is the only one considered relatively safe (FDA Category B), and even then, insulin is often preferred because it doesn’t cross the placenta. If you’re planning pregnancy or become pregnant, talk to your doctor immediately. You may need to switch from pills to insulin to protect your baby.
If you’re struggling with side effects, you’re not failing. You’re just human. Diabetes meds are powerful tools - but they’re not one-size-fits-all. The right one for you might not be the one your friend takes. Ask questions. Push for alternatives. Your body will tell you what it needs. Listen.