Medication Hemolytic Anemia Risk Checker
Medication Risk Checker
Enter a medication name to check for association with hemolytic anemia risk.
Risk Assessment
Important Action Steps
If you are experiencing symptoms like fatigue, shortness of breath, or yellowing of skin/eyes while taking this medication, contact your healthcare provider immediately.
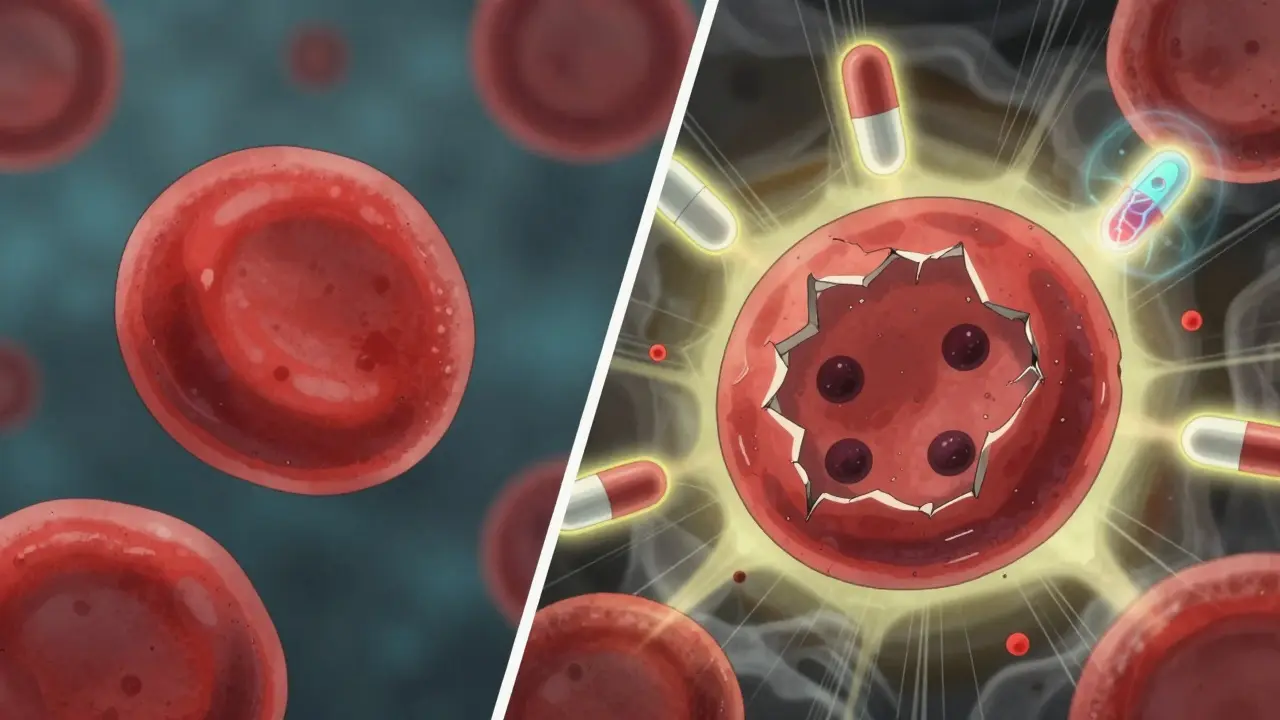
When a medication you’re taking starts killing your own red blood cells, it’s not just a side effect-it’s a medical emergency. Drug-induced immune hemolytic anemia (DIIHA) happens when your immune system, confused by a drug, attacks your red blood cells like they’re invaders. These cells normally live for about 120 days. In DIIHA, they’re destroyed in days-or even hours. The result? Severe fatigue, shortness of breath, yellowing skin, and sometimes heart failure. It’s rare, but when it happens, it’s serious. And most doctors don’t spot it right away.
How Medications Trigger Red Blood Cell Destruction
Not all drug-induced hemolysis works the same way. There are two main paths: immune-mediated and oxidative.
In immune-mediated DIIHA, the drug latches onto your red blood cells like a sticker. Your body sees this new combo as foreign and makes antibodies to destroy it. Think of it like a burglar putting on your neighbor’s jacket-your security system (your immune system) goes after the jacket, but ends up attacking your neighbor instead. The most common drugs that trigger this are cephalosporins, especially cefotetan, ceftriaxone, and piperacillin. Together, these antibiotics cause about 70% of immune-mediated cases.
The other path is oxidative hemolysis. Here, the drug doesn’t trick your immune system. Instead, it directly damages the hemoglobin inside red blood cells. This happens mostly in people with G6PD deficiency-a genetic condition that affects about 1 in 10 African American men and up to 1 in 7 men in Mediterranean regions. But even if you don’t have G6PD deficiency, some drugs can still cause this damage. Dapsone, phenazopyridine (Pyridium), nitrofurantoin, and even topical benzocaine sprays have been linked to this type of hemolysis. The damage creates clumps of broken-down hemoglobin called Heinz bodies, which rupture the cell from the inside.
Which Drugs Are Most Likely to Cause This?
It’s not just one or two bad actors. Over 100 medications have been tied to hemolytic anemia. But a few stand out.
For immune-mediated cases:
- Cefotetan
- Ceftriaxone
- Piperacillin
- Methyldopa (less common now, but historically significant)
- Penicillin and related antibiotics
- NSAIDs like ibuprofen or naproxen (rare, but documented)
For oxidative hemolysis:
- Dapsone
- Phenazopyridine (Pyridium)
- Nitrofurantoin
- Ribavirin
- Primaquine
- Sulfa drugs
- Topical benzocaine
- Amyl and butyl nitrate (“poppers”)
What’s tricky is that some drugs can cause both types. For example, nitrofurantoin can trigger immune-mediated hemolysis in some people and oxidative damage in others. And if you have G6PD deficiency, even a single dose of phenazopyridine can send your hemoglobin crashing within 24 hours.
What Does It Feel Like?
Early symptoms are easy to miss. They look like the flu, or just exhaustion. But if you’re taking one of these drugs and suddenly feel worse, pay attention.
Common signs include:
- Fatigue (92% of cases)
- Weakness (87%)
- Shortness of breath (76%)
- Rapid heartbeat (68% have heart rate over 100 bpm)
- Pale skin
- Yellow eyes or skin (jaundice, seen in 81%)
- Dark urine (from hemoglobin breakdown)
It can escalate fast. In acute cases, hemoglobin can drop 3 to 5 grams per deciliter in just 2 to 3 days. That’s like losing a full unit of blood overnight. For someone already anemic or elderly, this can trigger heart rhythm problems, heart muscle damage, or even heart failure. One study showed that 8% of patients with severe hemolysis developed heart failure when their hemoglobin fell below 6 g/dL.
How Doctors Diagnose It
There’s no single test. Diagnosis is a puzzle made of symptoms, timing, and lab results.
First, your doctor checks for signs of hemolysis:
- Elevated indirect bilirubin (>3 mg/dL)
- High LDH (>250 U/L)
- Low haptoglobin (<25 mg/dL)
Then they look at your blood under a microscope. Spherocytes (small, round red cells) suggest immune-mediated destruction. Heinz bodies (dark clumps inside red cells) point to oxidative damage.
The gold standard for immune-mediated DIIHA is the direct antiglobulin test (DAT). It finds antibodies stuck to your red blood cells. But here’s the catch: the DAT is positive in 95% of cases-but not always. If you’ve just started the drug, or if the drug binds weakly, the test can be negative. That’s why 43% of cases are missed at first.
If G6PD deficiency is suspected, testing is tricky. During active hemolysis, the test can give false negatives because it measures older red cells that are already destroyed. The enzyme levels in new cells (reticulocytes) look normal. So doctors wait 2 to 3 months after the episode to test accurately.
What Happens After Diagnosis?
The first and most important step? Stop the drug. Immediately.
Once the trigger is removed, most people start recovering in 7 to 10 days. Hemoglobin levels usually return to normal within 4 to 6 weeks. But that’s only if you catch it in time.
If your hemoglobin drops below 7-8 g/dL, or you’re having trouble breathing or your heart is racing, you’ll need a blood transfusion. It’s not just about replacing cells-it’s about preventing heart damage.
Some doctors still use steroids like prednisone. But studies show they don’t speed up recovery much. The body heals itself once the drug is gone. Steroids are only used if antibodies stick around after the drug is stopped.
For rare cases where the immune system keeps attacking even after stopping the drug, treatment gets stronger: intravenous immunoglobulins (IVIG), then drugs like rituximab, azathioprine, or cyclosporine. About 78% of these tough cases respond within 3 to 6 weeks.
If you have methemoglobinemia (a dangerous form of oxidative damage where blood can’t carry oxygen), methylene blue is the fix. But here’s the critical warning: never give methylene blue to someone with G6PD deficiency. It can cause massive hemolysis and death.
Why This Is Often Missed
Most doctors don’t think of DIIHA unless they’re hematologists. A 2024 study found that internal medicine residents correctly diagnosed DIIHA only 58% of the time on their first try. After training on the common drugs and lab patterns, that jumped to 89%.
Why? Because the symptoms look like everything else: infection, liver disease, other anemias. And the link between a common antibiotic and red blood cell death isn’t taught well in medical school.
Also, the delay matters. Immune-mediated DIIHA usually shows up after 7-10 days of taking the drug. So if you started a new antibiotic last week and now feel awful, your doctor might blame the infection, not the drug.
But oxidative hemolysis hits fast-within 24 to 72 hours. If you take phenazopyridine for a UTI and turn yellow the next day, that’s a red flag.
What You Can Do
If you’re on any of the high-risk drugs and feel unusually tired, short of breath, or notice yellowing skin, speak up. Ask: “Could this be related to my medication?”
If you’re of African, Mediterranean, or Southeast Asian descent, ask your doctor if you’ve ever been tested for G6PD deficiency. Many people don’t know they have it until they have a reaction.
Keep a list of all your medications-including over-the-counter and topical ones. That topical benzocaine spray you use for mouth sores? It’s on the list. So is the nitrofurantoin you took for a UTI last year. If you’ve had unexplained anemia before, tell your doctor. It might have been DIIHA.
Hospitals are starting to use electronic alerts that warn doctors when someone is prescribed a high-risk drug and has a history of hemolytic anemia. One study showed this cut severe cases by 32% in 18 months. That’s progress.
Looking Ahead
New treatments are on the horizon. Two clinical trials in 2024 tested drugs that block the immune system’s attack on red cells. Efgartigimod, used for myasthenia gravis, showed a 67% response rate in DIIHA patients. Complement inhibitors-drugs that stop the immune system from tearing cells apart-are also being studied.
But the best tool is still awareness. If you’re taking an antibiotic, a painkiller, or even a urinary tract medication and suddenly feel worse, don’t assume it’s normal. Your red blood cells are dying. And they need you to act fast.
Recovery is possible. But only if the drug is stopped before your heart or kidneys are damaged. Know the signs. Know the drugs. And if something feels wrong-trust it.
Can over-the-counter drugs cause hemolytic anemia?
Yes. Even common OTC drugs like phenazopyridine (Pyridium) for urinary discomfort or topical benzocaine in numbing sprays can trigger oxidative hemolysis, especially in people with G6PD deficiency. NSAIDs like ibuprofen have also been linked to immune-mediated cases, though rarely. Always check with your doctor before taking new medications if you’ve had unexplained anemia before.
Is hemolytic anemia from drugs more dangerous in older adults?
Yes. Older adults are at higher risk for complications because their hearts are less able to handle sudden drops in oxygen. A rapid hemoglobin drop below 7 g/dL can trigger arrhythmias or heart failure in people over 65, even if they had no prior heart issues. They’re also more likely to be on multiple medications, increasing the chance of a dangerous interaction.
How long does it take to recover after stopping the drug?
Most people start improving within 7-10 days after stopping the drug. Hemoglobin levels usually return to normal within 4 to 6 weeks. Full recovery of red blood cell production can take longer if the bone marrow was suppressed, but this is rare. The key is stopping the drug early-delaying increases the risk of permanent organ damage.
Can you get hemolytic anemia from vaccines?
There are extremely rare case reports of immune hemolytic anemia after vaccines, but no proven causal link. The risk is far lower than from antibiotics or other medications. If it happens, it’s typically linked to immune system overreaction, not the vaccine components themselves. The benefits of vaccination vastly outweigh this theoretical risk.
Should I get tested for G6PD deficiency if I’ve had unexplained anemia?
Yes. If you’ve had sudden anemia after taking a drug like dapsone, phenazopyridine, or sulfa antibiotics-and you’re of African, Mediterranean, or Southeast Asian descent-you should be tested. Wait 2-3 months after the episode for an accurate result. Knowing your G6PD status can prevent life-threatening reactions in the future.
Are children at risk for drug-induced hemolytic anemia?
It’s rare in children, but when it happens, it’s often more severe. Studies show pediatric cases present with lower hemoglobin levels (average 5.2 g/dL) compared to adults (6.8 g/dL). Kids can’t always describe symptoms like fatigue or jaundice, so parents and doctors need to be extra alert for sudden pallor, dark urine, or unexplained irritability after starting a new medication.

14 Comments
i had no idea some antibiotics could do this. my mom was on ceftriaxone last year and kept saying she felt like she was running on empty. we thought it was just aging... now i'm scared to even take ibuprofen.
g6pd def is real. my cousin in hyderabad got sick after taking sulfa for a UTI. they thought it was malaria at first. took 3 days to figure out it was the meds. dont ignore dark pee.
It is deeply concerning that pharmaceutical companies continue to market drugs without adequately testing for hemolytic potential in genetically diverse populations. This is not just negligence-it’s a systemic failure of medical ethics.
People really need to stop self-diagnosing. If you're taking meds and feel weird, call your doctor-not Reddit. This post is just fearmongering with a side of medical jargon.
The pathophysiological cascade initiated by drug-induced immune hemolysis involves complement-mediated erythrocyte lysis, resulting in a marked elevation of unconjugated bilirubin, lactate dehydrogenase, and a concomitant decrease in haptoglobin-hallmarks of extravascular hemolysis.
If you’re on any of these meds and not getting tested, you’re playing Russian roulette with your organs. Stop being lazy. Get your labs done. Your heart doesn’t care how busy you are.
Why is this even a thing in America? In India, they just tell you to stop the drug and you’re fine. Here, we turn every side effect into a lawsuit waiting to happen.
I appreciate the info but I wish there was a clearer warning on the pill bottles. I’ve taken nitrofurantoin three times and never knew it could do this. Just a little box on the label could save lives.
This is why we need global awareness. G6PD deficiency is common in South Asia, but most doctors here don’t screen for it unless you’re visibly jaundiced. We need better training, not just better drugs.
Wow. A whole 1000 words about how drugs can kill you. Groundbreaking. Next up: 'Water Can Cause Drowning: A Terrifying Revelation'.
THEY PUT POISON IN PILLS AND CALL IT MEDICINE?!?!? 😭💔 I took phenazopyridine for a UTI and my urine looked like cherry soda for 2 days. I thought it was ‘normal’ because the label didn’t say ‘DANGER’ in neon letters. I’m never trusting Big Pharma again. #RIPMyRedBloodCells
I wonder how many cases go undiagnosed because symptoms look like the flu or just 'being tired.' Maybe we need routine CBCs for people on long-term meds, not just when they’re already crashing.
if you’re on one of these meds and feel off, stop and get blood work. no drama. no panic. just check. your body tells you when something’s wrong. listen.
I had no idea about benzocaine sprays!! 😱 I used one for a sore throat last winter and felt weird for days. Now I get it. I’m deleting all my OTC sprays. 💔🩸
Write a comment