If your medication isn’t doing what it’s supposed to, you’re not alone. About half of all people don’t take their prescriptions as directed, and a big reason? They don’t feel like it’s helping. But instead of stopping cold or suffering in silence, there’s a better way: ask for alternatives. Talking to your doctor about what’s not working isn’t being difficult-it’s part of good care. In fact, studies show patients who speak up are over three times more likely to get unnecessary meds stopped safely. The key isn’t just asking-it’s asking the right way.
Before Your Appointment, Get Organized
Don’t walk into your doctor’s office hoping to remember everything. Most visits are short, and if you’re vague, your concerns might get brushed aside. Start by writing down exactly what’s happening.- When did the medication stop working? Did it help at first, then fade?
- What symptoms are still bothering you? Be specific: "My knee still hurts when I walk up stairs," not "It still hurts."
- What side effects are you noticing? Dizziness? Sleepiness? Upset stomach? Write down when they happen and how bad they are.
- Have you missed doses? If so, why? Was it too expensive? Too confusing? Too many pills?
Bring your actual medicine bottles. A 2022 study found that patients who did this reduced medication errors by 22%. Your doctor might spot interactions or dosing issues you didn’t even know about. Don’t forget to include over-the-counter meds, vitamins, and supplements-these can mess with your prescription too.
Use These Exact Questions to Start the Conversation
Words matter. Instead of saying, "This isn’t working," try this:- "Why am I taking this medication?"
- "What are the benefits and risks of staying on it?"
- "Are there other options I could try?"
- "Could any of these alternatives help with my main concern-like sleep, pain, or anxiety-without the side effects?"
- "Can I reduce the dose or stop it completely?"
These aren’t just random questions. They come straight from the Deprescribing Network, a Canadian-led group that’s helped over 47 U.S. health systems improve how meds are reviewed. Patients who used these questions saw more real conversations and fewer unnecessary prescriptions.
Also, don’t be afraid to say: "I’d like to understand what else might work." Or: "I’m worried about long-term use. Is there a different approach?"
Be Clear About Your Goals
Not all meds are created equal-and neither are your priorities. If you’re taking something for anxiety, maybe you care more about feeling calm during meetings than sleeping through the night. If you’re on a pain med, maybe you want to walk your dog without wincing, not just lower a number on a scale.One patient on Reddit shared: "I brought a two-week log of my pain levels before and after my pill. My doctor switched me right away to a different class of drugs-and it actually worked." That’s the power of specifics. Your doctor can’t guess what matters to you. Tell them.
Ask About Non-Medication Options
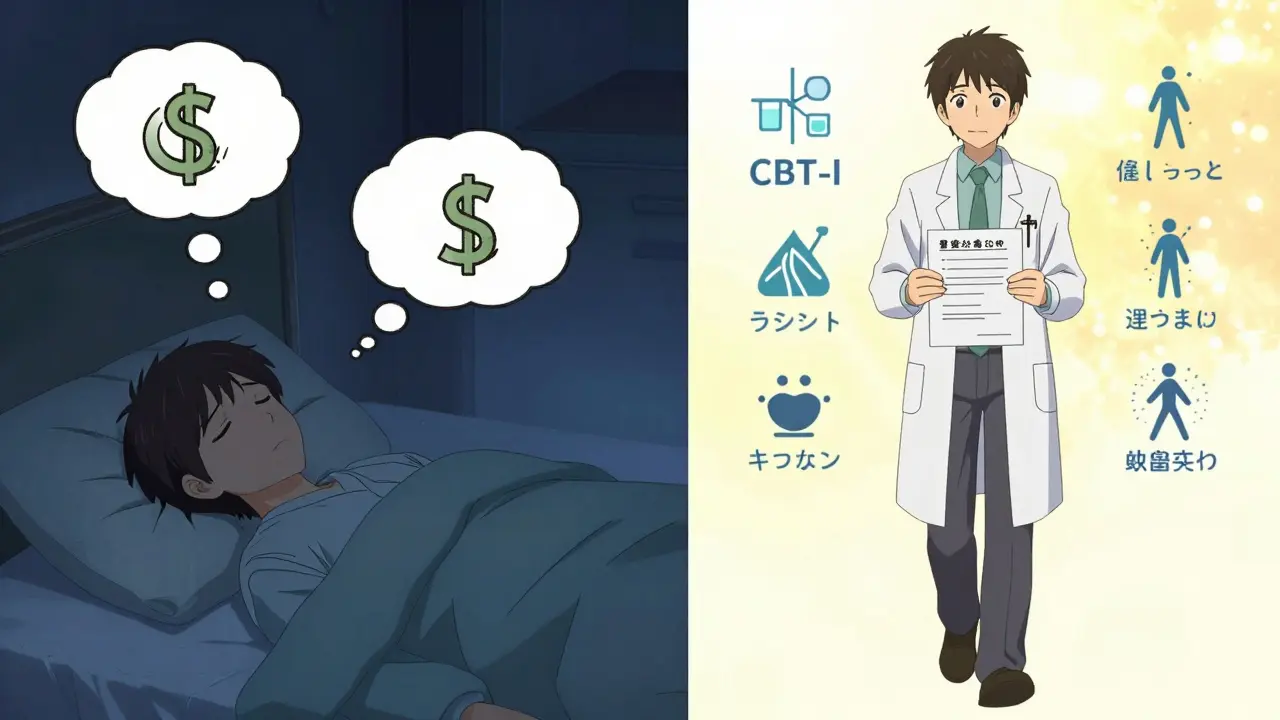
Medication isn’t the only tool. Sometimes, the best alternative isn’t another pill-it’s a change in lifestyle or therapy.- For sleep problems: Cognitive behavioral therapy for insomnia (CBT-I) works as well as sleeping pills after 8 weeks-and without the risk of falls or memory issues.
- For type 2 diabetes: Regular walking, eating whole foods, and losing even 5% of body weight can lower blood sugar as much as metformin in many people.
- For acid reflux: Cutting back on coffee, spicy food, and late-night snacks, plus using antacids like Tums or Rolaids, helped over half of people stop needing stronger meds.
- For back pain: Exercise, physical therapy, and acupuncture are now first-line recommendations by the American College of Physicians-better than NSAIDs for many, with fewer side effects.
- For anxiety: CBT and mindfulness practices match the effectiveness of SSRIs for mild to moderate cases, according to a 2022 Lancet review.
Ask: "Are there non-drug options I could try alongside or instead of this?" Many doctors are trained to think in pills-but they’re not always told how powerful lifestyle changes can be. Your question might open the door.
Bring Up Cost and Accessibility
If the medication isn’t working and it’s too expensive, you’re stuck in a bad spot. Don’t assume your doctor knows your budget. Say it outright:- "Is there a generic version?"
- "Is there another drug that works the same but costs less?"
- "Can you help me find a patient assistance program?"
AARP found that 62% of people who asked about cheaper alternatives got a switch to an affordable option. Generic drugs are often identical in effect but cost a fraction. And some programs help cover co-pays for brand-name meds if you qualify.
Request Written Instructions
If your doctor suggests a new medication or changes your regimen, ask for it in writing. MedlinePlus reports that patients who get written instructions understand their treatment 40% better than those who only hear it verbally.Also, ask: "What should I watch for?" and "When should I call back if things don’t improve?" This isn’t being paranoid-it’s planning ahead. Knowing what to expect helps you decide if the new option is working or if you need to go back to the drawing board.
What If Your Doctor Says No?
Sometimes, you’ll get a flat "no"-or worse, a dismissive comment like, "You’re just being difficult." That’s not okay. You have the right to be heard.- Ask: "Can you explain why this is the best option for me?"
- Request a referral to a specialist or pharmacist who focuses on medication reviews.
- Ask for a second opinion. Many insurance plans cover this.
- Use your patient portal to send a follow-up message. Sometimes, doctors respond better in writing.
One patient on a health forum wrote: "Asking, ‘Is this medication still necessary?’ led to me getting off three pills I didn’t need anymore." That kind of clarity doesn’t come from silence.

Use Technology to Your Advantage
Many health systems now offer tools to help. Epic Systems, used by over 60% of U.S. hospitals, has a feature called MyMedList that lets you type in medication concerns directly in your portal before your visit. Your doctor sees it ahead of time and comes prepared.Also, check if your pharmacy app has a "medication review" option. Some even flag possible side effects or interactions before you even walk in.
Don’t Wait Until Your Next Appointment
A 2022 study found that 32% of people waited until their next scheduled visit to mention a medication problem. That’s weeks of unnecessary discomfort-or worse, risk. Call your clinic. Send a message. Use the portal. You don’t need to wait. Many offices have nurses or pharmacists who can help adjust meds over the phone.If you’re in pain, dizzy, or having a bad reaction, don’t wait. Call immediately. Your safety comes before appointment slots.
Why This Matters More Than You Think
Taking the wrong med-or the right med at the wrong dose-can lead to falls, memory loss, hospital stays, and even death, especially for older adults. The National Institute on Aging says better communication cuts adverse drug events by 30% in seniors.And it’s not just about safety. When you understand your treatment and help shape it, you’re 35% more likely to stick with it. That’s not magic-it’s science. You’re not just a patient. You’re a partner in your care.
Medication isn’t a one-size-fits-all fix. What works for someone else might not work for you. And that’s okay. The system is designed to let you speak up. Use it.
What should I do if my medication isn’t working but my doctor won’t change it?
If your doctor refuses to consider alternatives, ask for a clear reason based on your health history. Say, "Can you explain why this is the only option?" If you’re still not satisfied, request a referral to a specialist, like a geriatrician or pharmacist who focuses on medication reviews. You can also ask for a second opinion-many insurance plans cover this. Don’t feel guilty for advocating for your health.
Can I stop my medication on my own if it’s not working?
Never stop a prescription suddenly unless your doctor tells you to. Some meds, like antidepressants, blood pressure pills, or steroids, can cause serious withdrawal effects or rebound symptoms. Instead, ask your doctor how to safely taper off or switch. They can guide you through a safe transition.
How long should I wait before deciding a medication isn’t working?
It depends on the drug. Some, like antibiotics, work in days. Others, like antidepressants or thyroid meds, can take 4 to 8 weeks. Ask your doctor upfront: "How long should I wait before we reassess?" That sets a clear timeline. If you’re still not better after that time, it’s time to talk about alternatives.
Are natural remedies or supplements good alternatives to prescription drugs?
Some supplements can help, but they’re not always safe replacements. For example, melatonin can help with sleep, but it doesn’t replace a sleep disorder diagnosis. St. John’s Wort may help mild depression, but it can interfere with birth control, blood thinners, and other meds. Always tell your doctor what you’re taking-even "natural" stuff. It’s not an alternative unless it’s been studied and approved for your condition.
Can pharmacogenomic testing help me find a better medication?
Yes. Pharmacogenomic testing looks at your genes to see how your body processes certain drugs. It’s already helping 57% of patients find better-fitting meds, especially for depression, pain, and heart conditions. Ask your doctor if this test is right for you. It’s not routine yet, but it’s becoming more common-and insurance is starting to cover it in some cases.
What if I can’t afford the alternative medication?
Always ask: "Is there a generic version?" or "Can you help me find a discount program?" Many drugmakers offer patient assistance programs. Pharmacies like CVS, Walgreens, and Walmart have $4 generic lists for common meds. Also, check with local health clinics-they often have free or low-cost medication programs. You don’t have to choose between health and affordability.
How do I know if a new medication is actually working?
Set a clear goal and timeline. For example: "I want to sleep 6 hours a night without waking up" or "I want to walk 20 minutes without pain." Track it daily for 2-4 weeks. If you’re not seeing progress by then, schedule a follow-up. Don’t just assume it’s "taking time." If it’s not helping after the expected window, it’s time to try something else.
Next Steps: What to Do Today
- Look at your medicine cabinet. Write down every pill, vitamin, and supplement you take.
- Identify one medication that isn’t working the way it should.
- Write down three specific concerns about it: symptoms, side effects, or cost.
- Call your doctor’s office and ask: "Can I schedule a 20-minute medication review?"
- Bring your list and bottles to the appointment.
You’re not asking for a favor. You’re asking for care that fits you. That’s not just reasonable-it’s your right.

13 Comments
Man, I wish I’d known all this two years ago when I was just powering through that awful antidepressant that made me feel like a zombie. I didn’t even realize I could ask for alternatives-I just thought, ‘Well, this is just how it is.’ Turns out, my doctor was totally fine switching me once I showed up with a list of side effects and my actual pill bottles. No judgment, just a nod and a ‘Let’s try this instead.’ Life changed.
Now I bring my supplements too. Turns out, that ‘natural’ ashwagandha I was taking was messing with my blood pressure med. Who knew? My doctor didn’t, until I showed her the bottle. Now I’m on a better med, I sleep like a baby, and I don’t feel like I’m floating through life.
Also, the part about writing down goals? Huge. I wrote, ‘I want to play with my niece without being exhausted by 3 PM.’ She laughed and said, ‘Okay, that’s your new metric.’ We swapped meds. Worked.
Don’t wait till you’re miserable. Just ask. It’s not being difficult. It’s being smart.
And yes, I still bring my pill bottles. No shame.
It is imperative to underscore the clinical and ethical necessity of patient-centered pharmacotherapy. The evidence presented herein aligns with the tenets of shared decision-making as articulated by the Institute of Medicine in 2001, and further reinforced by the 2020 Cochrane Review on deprescribing. The structured communication framework proposed-particularly the use of targeted, evidence-based inquiry-is not merely advisable; it is a standard of care.
Moreover, the inclusion of over-the-counter agents and dietary supplements in medication reconciliation is not ancillary-it is foundational. Failure to document these constitutes a breach in the duty of care. The 22% reduction in medication errors observed in the 2022 study is not an anomaly; it is a reproducible outcome of rigorous documentation.
I urge all clinicians to institutionalize this protocol. And I implore patients: do not hesitate to request written documentation. Verbal instruction alone is insufficient for safe, sustainable care.
Oh honey, let’s get real for a sec-medication isn’t some magic spell you whisper to a white coat and expect miracles. It’s a biological negotiation between your DNA, your trauma, your coffee habit, and the pharmaceutical industry’s quarterly earnings report.
I once took a drug that was supposed to ‘stabilize my mood’ but instead turned me into a sobbing blob who cried during dog commercials. I asked for alternatives. My doctor said, ‘Maybe try yoga?’ I said, ‘I’ve been doing yoga since 2014 and my therapist still calls me ‘the human emotional storm.’’
So I dug into pharmacogenomics. Turned out my liver metabolizes SSRIs like a toddler eats broccoli-slowly, messily, with lots of drama. Switched to a different class. No more crying at puppies. Now I’m just mildly annoyed at them. Progress.
Also, ‘natural remedies’? Please. If your ‘herbal solution’ has a TikTok influencer holding a bottle like it’s the Holy Grail, run. Not because it’s fake-but because it’s unregulated chaos dressed in lavender.
Speak up. Bring your bottles. Write it down. Your body isn’t a beta test. It’s your only one.
Wow. Just... wow. You people actually think doctors are here to help? Ha. They’re paid by Big Pharma to keep you on pills. You think they want you to stop? They want you addicted. They want you on three meds so they can bill Medicare for ‘medication management.’
And don’t even get me started on ‘CBT-I’-that’s just government brainwashing disguised as therapy. Sleep? Take a pill. That’s what my grandfather did. He lived to 92. He didn’t sit around journaling about his ‘sleep hygiene.’ He took his pill and slept.
And why are you even asking about generics? You think the government wants you to save money? No. They want you on the brand name so they can track you. Surveillance. That’s what this is.
Just take the pill. Don’t question. Don’t write lists. Don’t bring bottles. Just obey. That’s what you’re supposed to do.
And if you’re still sick? Maybe it’s your attitude. Maybe you’re not praying enough.
I’ve been on three different blood pressure meds in the last five years. Each time, I felt like I was asking for too much. Like I was being a burden. But after my last appointment-where I showed up with a notebook, my pill bottles, and a list of times I felt dizzy-I realized my doctor wasn’t annoyed. She was impressed.
She said, ‘I wish more patients came in like this.’
It’s not about being difficult. It’s about being present. You’re not asking for special treatment-you’re asking for your health to matter. And it does.
Bring the list. Bring the bottles. Bring your truth. They’re not going to fire you for caring too much. They’re going to thank you for showing up.
Let’s be real-this whole ‘ask for alternatives’ thing is just a feel-good fantasy for people who don’t understand how medicine actually works.
Most ‘alternatives’ are just cheaper drugs the company wants to push next quarter. CBT-I? Works great if you have time, money, and a therapist who doesn’t charge $300/hour. Walking for diabetes? Cool. Unless you work two jobs and your apartment has no sidewalks.
And don’t get me started on ‘pharmacogenomic testing.’ It’s a $1,200 lottery ticket. 57% success rate? That means 43% of people wasted their money.
Also, why are we pretending doctors don’t have quotas? They’re pressured to ‘manage’ meds, not ‘explore’ them. If you think your two-minute visit is about your goals, you’re delusional.
This post reads like a pharmaceutical ad written by a wellness influencer. Real talk? Take the pill. Or don’t. But don’t pretend this is a system designed for you.
This is the kind of info I wish I had when I was 28 and terrified of my anxiety meds
I was so scared to say anything I just kept taking them and feeling like a ghost in my own life
Then one day I wrote down three things I wanted back-sleeping through the night, laughing without guilt, walking my dog without panic
My doctor didn’t blink. We switched. Now I’m on a lower dose and doing yoga twice a week
Don’t wait till you’re broken to speak up
You’re not being difficult
You’re being brave
And honestly? Your doctor probably wishes you’d asked sooner
Here’s the truth no one says: doctors are overworked, underpaid, and drowning in paperwork. That’s why they zone out during your 10-minute visit.
But here’s what you can do-you show up with a printed list. Not a note on your phone. Printed. On paper. With your meds labeled. With your symptoms bullet-pointed.
That’s the magic trick. That’s how you get their attention.
I did it last year. My doctor looked up from her screen, paused, and said, ‘I’ve never seen this before.’
She spent 25 minutes with me.
She changed my meds.
She gave me a referral.
You don’t need to be loud.
You just need to be prepared.
And if you’re scared? Bring a friend. Or write it down and read it out loud. Your voice matters. Even if it shakes.
Let’s not sugarcoat this-America’s healthcare system is a broken, profit-driven machine. You think your doctor cares about your ‘goals’? They care about meeting their HEDIS metrics and avoiding malpractice claims.
And this talk about ‘non-medication options’? Cute. But tell that to the single mom working two shifts who doesn’t have time for CBT-I or acupuncture. She needs a pill that works now.
Also, why are we pretending this isn’t a class issue? The people writing these articles? They have insurance, paid time off, and a therapist on speed dial.
Meanwhile, I’m on Medicaid, trying to get a $4 generic that’s out of stock because the manufacturer stopped making it.
Stop pretending this is about ‘patient empowerment.’ It’s about surviving a system that doesn’t care.
They want you to ask questions? That’s what they want. So you think you’re smart. But you’re being manipulated. The government wants you to think you have control. But they’re the ones who approve every drug. Every test. Every ‘alternative.’
They’re not letting you choose. They’re guiding you to the choices they want you to make.
And why do you think they push ‘generic’ so hard? Because it’s cheaper. Not better. Just cheaper. So they can save money on your healthcare and use it to fund something else.
Don’t fall for it. Just take the pill they give you. Don’t ask. Don’t bring bottles. Don’t write lists.
They don’t want you to think. They want you to obey.
And if you do? You’ll live longer. Because you’re not fighting the system.
You’re just surviving it.
It is my professional opinion, grounded in decades of clinical observation and adherence to international standards of medical ethics, that the framework outlined herein represents a paradigmatic shift toward patient autonomy in pharmacological decision-making.
Moreover, the integration of pharmacogenomic testing into routine practice-while not yet universally accessible-constitutes a necessary evolution in precision medicine. The 57% efficacy rate cited is not merely statistically significant; it is clinically transformative.
I would further recommend that all healthcare institutions implement mandatory training modules on deprescribing protocols, with certification for providers who demonstrate competency in patient-centered medication review.
And let us not overlook the critical role of pharmacy-based medication reconciliation services, which, when properly resourced, reduce hospital readmissions by up to 18% in elderly populations.
This is not advocacy. This is best practice.
CBT-I is gold standard for insomnia-no debate. But here’s the kicker: access is a nightmare. If you’re in rural Ohio or the Bronx, good luck finding a provider who takes your insurance.
And don’t get me started on ‘lifestyle changes’ as alternatives. Sure, walking helps diabetes. But what if you work nights? What if your neighborhood’s unsafe after 6? What if you’re on SSI and can’t afford the gym membership?
Don’t shame people for needing meds. The system failed them first.
Advocacy is good. But policy change is the real alternative.
Until then? Take the pill. Ask for the generic. Bring the bottles. And keep showing up.
Because the system won’t fix itself.
But you? You can still fight for your body.
Wait, I just read your comment about ‘the system won’t fix itself’-and I’m crying a little. That’s exactly what I felt when I got off that last med.
I didn’t think I had the right to ask. I thought I was just ‘difficult.’
But then I remembered: I’m not a patient. I’m a human with a body, a life, and a right to feel okay.
So yeah. Bring the bottles. Write the list. Say the hard thing.
Because if we don’t speak up, who will?
Thanks for saying that. I needed to hear it.
Write a comment