Every year, over 1.3 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t caused by bad prescriptions or pharmacy errors-they happen because people are taking too many pills, eating the wrong foods, skipping sleep, or sitting too much. The good news? You don’t need to rely on more drugs to fix the problem. Often, the solution is simpler than you think: lifestyle changes.
Why Lifestyle Changes Matter More Than You Think
Medications are powerful tools. But they don’t fix the root cause of most chronic conditions. High blood pressure? Diabetes? High cholesterol? These aren’t random glitches-they’re signs your body is out of balance. Drugs manage symptoms. Lifestyle changes fix the problem. A 2023 study in JAMA Internal Medicine looked at over 3.4 million people and found that when people made consistent lifestyle changes, they cut their need for medications by 25% to 50%. That’s not a small win. That’s life-changing. For someone on five or more pills a day-what doctors call polypharmacy-the risk of dangerous side effects jumps by 300%. Reducing that number isn’t just about saving money. It’s about staying out of the hospital.Move More: The Quiet Miracle for Blood Pressure and Blood Sugar
You don’t need to run marathons. You don’t even need a gym membership. Just walking briskly for 30 minutes, three times a week, can make a real difference. Research from JenCare Medical Centers shows that regular walking helps your heart pump more efficiently. That means your blood pressure drops naturally. In one case, a patient in Halifax went from 150/95 to 125/80 after six months of daily walks and cutting salt. His doctor took him off one blood pressure pill. For people with Type 2 diabetes, movement works even better. Losing just 5-7% of your body weight through walking and light strength training can reduce the need for diabetes medication by up to 60% in prediabetic people and 40% in those already diagnosed. That’s not theory-it’s what happened in real clinics across the U.S., including in UC Davis’s wellness program. The key? Consistency. You won’t see results in a week. It takes 8-12 weeks of steady movement before your body starts responding. But once it does, the benefits stick.Eat Smarter: Food That Works Like Medicine
What you eat isn’t just fuel. It’s medicine-or poison, depending on what you choose. For high blood pressure, the DASH diet (Dietary Approaches to Stop Hypertension) is backed by the New England Journal of Medicine. It’s simple: more vegetables, fruits, whole grains, beans, nuts, and lean proteins. Less salt, sugar, and processed foods. Reducing sodium from 3,500 mg to 1,500 mg a day lowers blood pressure as much as a single pill. For diabetes, cutting refined carbs and sugar is the biggest game-changer. A diabetic-friendly plate-half non-starchy veggies, a quarter lean protein, a quarter whole grains-can control blood sugar as well as metformin in many cases. One patient in Michigan cut her A1C from 8.2 to 6.1 in nine months just by changing her meals. She stopped taking two pills. But here’s the catch: some healthy foods can interfere with meds. Grapefruit ruins the effect of 85% of statins. Spinach and kale, packed with vitamin K, can make blood thinners like warfarin less effective. Dairy can block antibiotics. That’s why you need to talk to your pharmacist before changing your diet. Not your friend. Not Google. Your pharmacist.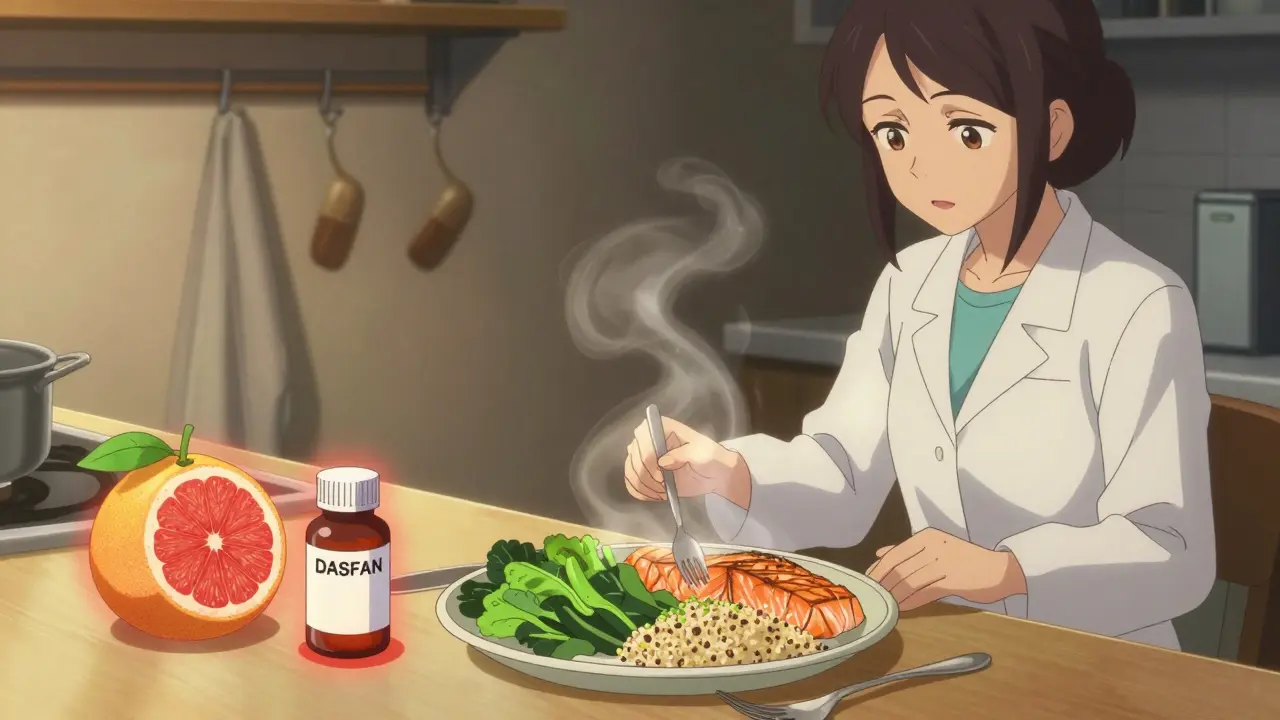
Sleep Like Your Life Depends on It-Because It Does
Most people don’t realize how much sleep affects their meds. If you’re sleeping less than seven hours a night, your body is under constant stress. That raises cortisol, spikes blood sugar, and increases blood pressure. It also makes your body less responsive to insulin and harder to lose weight. Studies show people who sleep poorly are 40% more likely to develop Type 2 diabetes. They’re also more likely to need higher doses of blood pressure meds. The fix? Set a bedtime. Turn off screens an hour before sleep. Keep your room cool and dark. No caffeine after 2 p.m. It’s not magic. It’s biology. Your body repairs itself while you sleep. If you’re not sleeping enough, you’re asking your meds to do double duty-and they can’t.Quit Smoking, Cut Alcohol, Manage Stress
Smoking is the worst thing you can do if you’re on heart meds. It damages blood vessels, raises blood pressure, and makes statins less effective. Quitting cuts your risk of heart attack by 50% in just one year. Alcohol is tricky. A drink or two a week might be fine. But daily drinking? It raises blood pressure, worsens liver damage from statins, and can cause dangerous drops in blood sugar if you have diabetes. The rule: one drink a day for women, two for men. And no bingeing. Stress is the silent killer. It spikes cortisol, which raises blood sugar and blood pressure. Yoga, meditation, even 10 minutes of deep breathing a day can lower stress hormones enough to reduce your need for meds. One study showed people who practiced mindfulness for eight weeks lowered their systolic blood pressure by 10 points-without changing their pills.Don’t Replace Meds-Support Them
This is the biggest mistake people make. They see a blog saying “You can beat diabetes without pills,” and they stop their meds. That’s dangerous. Harvard Medical School’s Dr. Rob Shmerling says it clearly: “Medications should be in addition to lifestyle changes, not instead of them.” Lifestyle changes take time. Medications work fast. If you stop your meds before your body adapts, you could have a stroke, a heart attack, or a diabetic emergency. The right approach? Work with your doctor. Start the lifestyle changes. Give it 3-6 months. Then, ask: “Can we lower my dose?” Not “Can I stop?”
What to Do Next: A Simple 30-Day Plan
You don’t need to overhaul your life overnight. Start small.- Week 1-2: Walk 20 minutes, three days this week. Cut out sugary drinks. Go to bed 30 minutes earlier.
- Week 3-4: Walk five days a week. Swap white bread for whole grain. Write down what you eat and sleep each day.
- Month 2: Talk to your pharmacist about food-drug interactions. Ask your doctor if you can reduce one medication dose after 60 days of consistent changes.
When to Call Your Doctor
Lifestyle changes are powerful-but not a substitute for medical care. Call your doctor if:- Your blood pressure spikes above 180/110
- You feel dizzy, confused, or unusually tired
- You have unexplained bruising or bleeding (could mean your blood thinner is too strong)
- You’re losing weight without trying
The Bigger Picture: This Isn’t Just About You
The cost of medications in the U.S. is over $1,000 per person per year. That’s $370 billion spent annually. Lifestyle medicine could cut that by billions. More than 12,000 doctors are now certified in lifestyle medicine. Medicare Advantage plans now cover nutrition coaching and exercise programs. Employers are seeing 18.7% lower healthcare costs when their staff follow these changes. This isn’t a trend. It’s the future of medicine. And you don’t have to wait for the system to catch up. You can start today-with a walk, a better meal, a good night’s sleep.Can lifestyle changes really replace my medications?
No, not on their own-at least not right away. Lifestyle changes take weeks or months to show results. Medications work fast. The goal is to use lifestyle changes to reduce your need for meds over time, under your doctor’s supervision. Never stop taking your pills without talking to your provider first.
How long until I see results from lifestyle changes?
It varies. Blood pressure can drop in 2-4 weeks with diet and walking. Blood sugar improvements often take 6-8 weeks. Weight loss and insulin sensitivity usually need 3-6 months of consistent effort. Don’t give up before the 60-day mark.
What foods should I avoid if I’m on medication?
Grapefruit interferes with 85% of statins. Leafy greens like spinach and kale can reduce the effect of warfarin. Dairy can block some antibiotics. Always check with your pharmacist before making big diet changes. They know exactly what foods interact with your specific meds.
Do I need to exercise every day?
No. The American Heart Association recommends 150 minutes of moderate exercise per week-that’s 30 minutes, five days a week. You can break it into 10-minute walks if needed. The key is consistency, not intensity. Walking counts.
Can I do this if I’m older or have mobility issues?
Absolutely. Seated exercises, water aerobics, stretching, and even short walks around the house count. The goal is movement, not fitness. A 10-minute walk after each meal helps blood sugar control. That’s enough to start. Talk to your doctor about safe options for your body.
Will my insurance cover lifestyle programs?
Many Medicare Advantage plans now cover nutrition counseling, exercise classes, and stress management programs. Private insurers are starting to follow. Ask your plan or your doctor’s office-they often have lists of covered programs in your area.
What if I can’t stick to the changes?
Most people struggle at first. It’s normal. Start with one tiny change: swap soda for water, or walk for 10 minutes after dinner. Build from there. Find someone to do it with-a friend, a family member. Progress isn’t linear. What matters is that you keep trying.
Reducing medication risks isn’t about being perfect. It’s about being consistent. It’s about choosing a walk over a pill, a vegetable over a snack, sleep over scrolling. These aren’t just habits. They’re your best defense against side effects, hospital visits, and long-term damage. Start small. Stay steady. Your body-and your meds-will thank you.
