Why Medication Management at Home Matters for Seniors
More than half of adults over 65 take at least five prescription drugs every day. Some take ten, fifteen, or even more. With so many pills, schedules, and possible side effects, it’s easy for mistakes to happen. A missed dose. A double dose. A drug interaction no one saw coming. These aren’t just small errors-they can land someone in the hospital.
That’s where home health services come in. These aren’t just helpers who drop off medicine. They’re trained professionals who manage the entire medication system at home. They check what’s prescribed, make sure nothing’s duplicated, confirm dosages match the doctor’s orders, and track whether the patient actually takes it. In fact, studies show that when professional medication management is used, adverse drug events drop by 60% compared to self-management.
For seniors recovering from surgery, a heart attack, or a stroke, this support isn’t optional-it’s lifesaving. One study found that patients using home health medication services had 20% fewer hospital readmissions within 30 days. That’s not just a number. It’s fewer emergency room trips, less stress for families, and more time spent safely at home.
What Exactly Do Home Health Services Do for Medications?
Home health nurses and aides don’t just hand out pills. They run a full medication safety system. Here’s what that looks like in practice:
- Medication reconciliation: They start by making a complete, up-to-date list of every medication the patient takes-brand names, generic names, doses, times, and why each one was prescribed. This list gets shared with every doctor, pharmacist, and specialist involved.
- Duplicate detection: One patient was taking two different blood pressure pills that did the exact same thing. The home health nurse caught it before the patient had a dangerous drop in blood pressure.
- Side effect monitoring: They watch for new symptoms like dizziness, confusion, or nausea. These aren’t just "old age" signs-they could be reactions to a new drug combo.
- Adherence tracking: They don’t assume the patient remembers to take pills. They log each dose taken, note missed doses, and flag patterns. If someone skips meds every Tuesday, they find out why.
- Emergency prep: They help create a simple, printed list of all medications and contacts, kept in a wallet or on the fridge. In an emergency, first responders don’t have to guess what’s being taken.
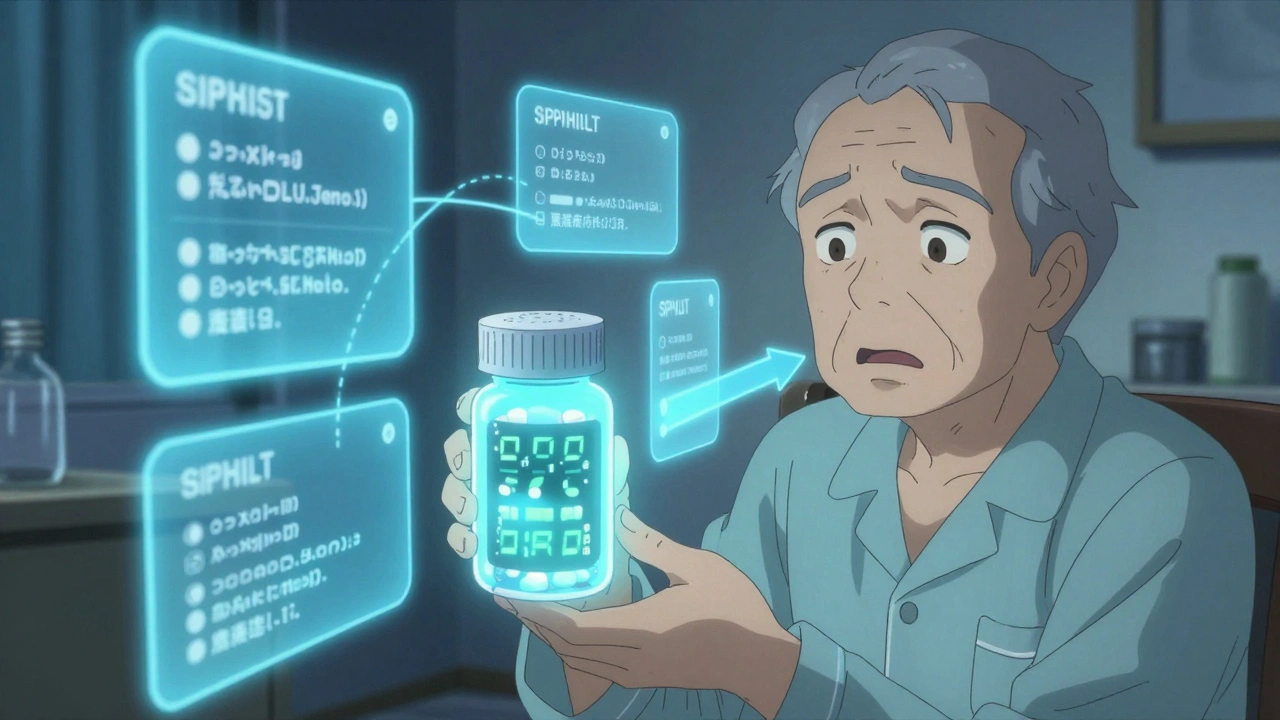
Tools That Make Medication Easier to Manage
Even with help, managing meds can be overwhelming. That’s why home health agencies use practical tools that work.
Pill organizers are the most common. Weekly or daily boxes with labeled compartments reduce errors by up to 45%. Some even have alarms built in. But not all are created equal. A simple plastic box won’t help someone with poor vision. Look for ones with large print, high-contrast colors, or even voice reminders.
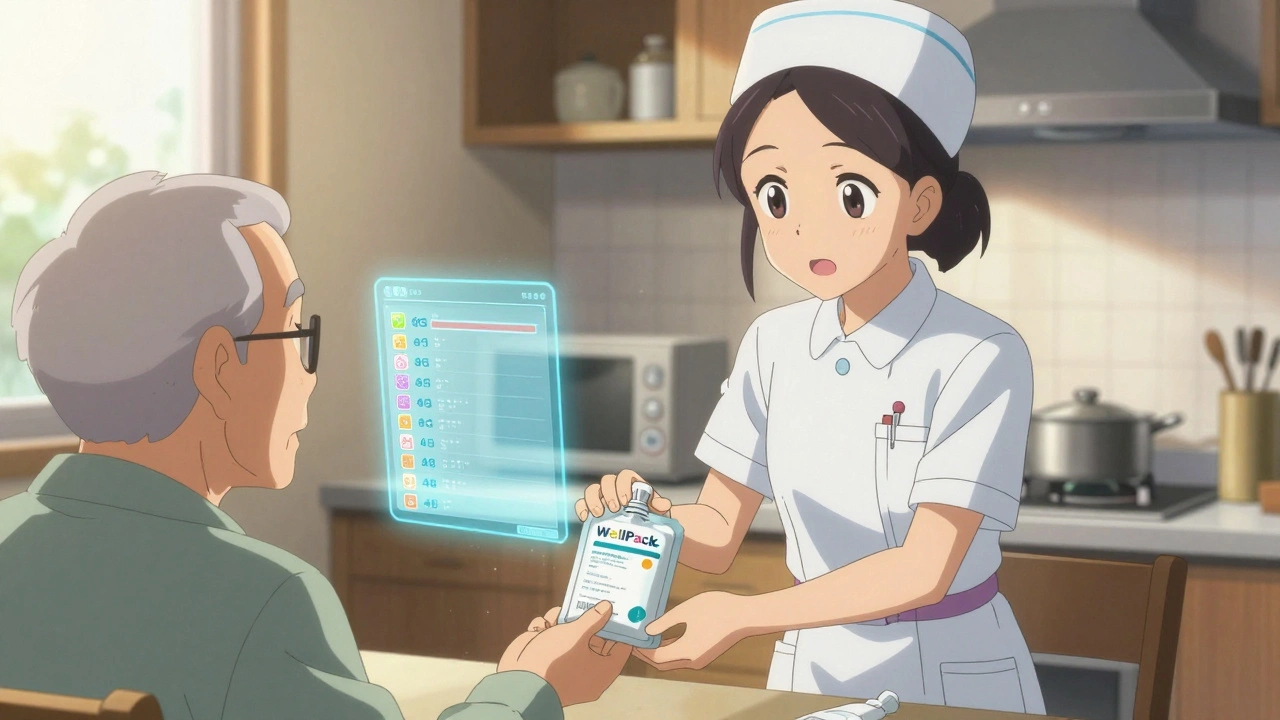
WellPack systems are another option. Instead of boxes, medications are sealed into individual daily pouches labeled with the time and date. Each pouch contains exactly what the patient needs for that moment-no sorting, no counting. This is especially helpful for people taking eight or more medications.
Digital apps are growing fast. Apps that send phone alerts, track doses, and even notify family members when a pill is skipped have improved adherence by 35%. Some newer ones use biometric verification-like a fingerprint scan-to confirm the right person took the right dose. In pilot programs, this cut administration errors by 40%.
And for non-English speakers, some agencies now include QR codes on pill pouches. Scan it, and a video plays in your language showing how to take the pill. That’s a game-changer for families who struggle to explain instructions.
Who Pays for Home Health Medication Services?
This is one of the biggest questions families face. The answer depends on who qualifies and what kind of care is needed.
If you’re enrolled in Medicare Part A, you may get home health services at no cost-if you meet specific criteria. You must be homebound, need skilled nursing care (like medication management), and have a doctor’s order. But here’s the catch: Medicare only covers intermittent visits. That means if you need help every day, you might not qualify.
Medicare Advantage plans are starting to cover more. Some now include daily medication monitoring, especially for people with chronic conditions like diabetes or heart failure. Check your plan’s benefits-this is changing fast in 2025.
Private home care agencies charge between $20 and $40 per hour for medication management. That adds up quickly if you need daily help. Some families combine services: use Medicare for skilled nursing visits twice a week, and hire a private aide for the other days.
There’s also long-term care insurance and state Medicaid programs that may cover home-based medication support. In Canada, provincial health plans often include home care services, but waitlists can be long. In Halifax, for example, eligibility is based on medical need, not income-but demand outpaces supply.
When Home Health Services Work Best (and When They Don’t)
Home health medication services aren’t a one-size-fits-all solution. They shine in certain situations-and fall short in others.
Best for:
- Post-hospital discharge: After a fall, heart surgery, or infection, seniors are at highest risk for medication errors. Home health teams help bridge the gap between hospital and home.
- Polypharmacy: Anyone taking five or more medications benefits from professional oversight. Drug interactions multiply with each added pill.
- Cognitive changes: If someone forgets doses, gets confused about schedules, or can’t read labels, a home health worker provides essential structure.
- Language or literacy barriers: When instructions are hard to understand, visual aids and translated videos make a huge difference.
Limited in:
- Psychiatric medications: Drugs for depression, anxiety, or psychosis often need frequent dose changes. Home health staff can’t adjust these-they can only administer them. A psychiatrist’s direct involvement is still needed.
- 24/7 needs: If someone needs help at 3 a.m. every night, most agencies can’t provide that level of coverage. Private duty nursing is an option, but it’s expensive.
- Uncooperative patients: If someone refuses to take meds or hides them, no amount of organization will help. Behavioral support may be needed too.
How to Get Started with Home Health Services
Getting help isn’t as complicated as it seems. Here’s how to begin:
- Ask your doctor. Say: "I’m worried about my parent’s medications. Can you refer us to a home health agency?" They’ll need to write an order for skilled nursing services.
- Check Medicare eligibility. Go to medicare.gov or call 1-800-MEDICARE. Ask: "Does this person qualify for home health under Part A?"
- Compare agencies. Look for ones certified by Medicare and licensed by your state. Ask if they use pill organizers, digital tools, and have staff trained in geriatric medication safety.
- Ask about their process. Do they do medication reconciliation on the first visit? Do they update the list after every doctor’s appointment? Do they use teach-back methods to confirm understanding?
- Start small. Begin with two visits a week. See how it works. Adjust as needed.
What to Watch Out For
Not all home health agencies are the same. Here are red flags:
- No medication list update. If they don’t ask for new prescriptions or changes, they’re not doing their job.
- Staff who don’t use teach-back. They should ask the patient to repeat instructions in their own words. "Tell me how you’ll take this pill tomorrow." If they skip this, errors will happen.
- Delayed documentation. CMS requires medication changes to be documented within 24 hours. If they’re late, it’s a sign of poor systems.
- No emergency plan. They should leave a printed, easy-to-read list of meds and contacts. If they don’t, ask why.
On the flip side, look for agencies that use QR codes, biometric verification, or multilingual resources. These show they’re investing in real safety-not just checking boxes.
Real Stories: What Families Are Saying
Mary K. from Ohio started using Phoenix Home Care’s WellPack system after her mother missed 30% of her doses. Within two weeks, missed doses dropped to under 5%. "It’s like they took the chaos out of medicine time," she said.
John T. from Michigan wasn’t so lucky. His father was on blood thinners, and two different doctors prescribed overlapping medications. The home health nurse didn’t catch it. His father ended up in the ER with internal bleeding. "They were supposed to check for interactions," John said. "They didn’t."
A Clarest survey of 500 caregivers found 78% saw better adherence with professional help. But 42% said coordinating between multiple doctors was a nightmare. That’s why medication reconciliation isn’t just a task-it’s a conversation that needs to happen between all providers, and the family needs to be part of it.
What’s Changing in 2025
Home health is evolving fast. By the end of this year, 65% of agencies are expected to use AI tools that scan for dangerous drug interactions in real time. That’s huge. Instead of waiting for a side effect to show up, the system flags risks before the pill is even taken.
Medicare Advantage plans are expanding coverage for continuous monitoring devices-like smart pill bottles that log when opened. Some now cover these as part of chronic care programs.
But there’s a problem: home health nurses are in short supply. One in four positions in Canada and the U.S. is vacant. That means longer wait times and overworked staff. If you’re using a service, ask how often the same nurse visits. Consistency matters.
Final Thought: It’s Not About Control-It’s About Safety
Many seniors don’t want help because they fear losing independence. But medication management isn’t about taking control. It’s about giving them more control over their health. Fewer hospital visits. Fewer side effects. More mornings where they feel okay.
The goal isn’t to manage every pill. It’s to make sure the right pills are taken at the right time-so the person can live, not just survive.
Can home health services give my parent their medications?
Yes, licensed home health nurses and trained aides can administer medications as prescribed. They don’t decide what’s given-they follow the doctor’s orders. They also document each dose and watch for reactions. But they can’t adjust doses or prescribe new ones-that’s still the doctor’s job.
Is home health medication management covered by Medicare?
Medicare Part A covers home health medication services if you’re homebound and need skilled nursing care. But it’s intermittent-usually a few times a week, not daily. If you need daily help, you may need to pay out of pocket, use Medicaid, or get coverage through a Medicare Advantage plan.
What’s the difference between a home health nurse and a home care aide?
A home health nurse is a licensed professional (RN or LPN) who can assess health status, administer injections, manage IVs, and handle complex medication regimens. A home care aide helps with daily tasks like bathing, dressing, and meal prep. Some aides are trained to remind about pills, but only nurses can actually give them.
How often should medication lists be updated?
Every time there’s a change-new prescription, discontinued drug, dose adjustment, or doctor visit. The Centers for Medicare & Medicaid Services require agencies to reconcile medications at every care transition. Best practice is to review the list monthly and after every hospital or clinic visit.
Can I use a pill organizer instead of home health services?
A pill organizer helps, but it’s not enough on its own. It doesn’t catch duplicate prescriptions, drug interactions, or side effects. It also doesn’t document missed doses or alert a professional if something’s wrong. For complex regimens or cognitive issues, professional oversight is necessary for safety.
What should I do if my parent refuses to take their meds?
Don’t force it. Talk to the home health nurse or doctor. Sometimes refusal is due to side effects, confusion, or fear. The nurse can help identify the cause-maybe the pill tastes bad, or they’re worried about addiction. Adjustments can be made, or alternative forms (like liquids or patches) can be explored. Behavioral support may also be needed.
8 Comments
Let’s be real-polypharmacy is a pharmacokinetic nightmare without structured medication reconciliation. The 60% reduction in ADEs isn’t anecdotal; it’s backed by JAMA meta-analyses. If your agency isn’t doing real-time CDS integration with EHRs, you’re just rearranging deck chairs on the Titanic.
Wow. Finally someone who gets it. 🙄 Most families think a pillbox = safety. Nope. It’s like giving a chainsaw to a toddler and calling it 'tool literacy.' If you're not using biometric verification and AI-driven interaction alerts, you're not managing meds-you're gambling with Grandma's life.
There’s something deeply human here, beyond the protocols and the pill organizers. It’s not just about avoiding hospitalizations-it’s about preserving dignity. When someone can take their own pills without being reminded, without feeling like a burden, without the shame of forgetting-that’s when care becomes truly healing. The tools matter, yes. But the presence of someone who notices you skipped your Tuesday dose… and asks why… that’s the medicine that lasts.
so true about the wellpack system… i saw my uncle use it after his stroke. no more confusion. but the real win? when the nurse sat with him for 20 mins just explaining why each pill mattered. not just handing out pouches. that’s care. 🙏
QR codes in local language. That’s the future. Simple. Smart. No bureaucracy. Just understanding.
Oh sweetie. You really think a $40/hour aide is going to catch a drug interaction? Honey, the nurse who showed up at my mom’s house didn’t even know what 'warfarin' meant. She just asked if she 'needed a nap.' 😂
Medicare only covers 'intermittent' visits? That’s a joke. My dad needs daily help and they told him to 'get a family member.' So I quit my job. Now I’m broke, exhausted, and still can’t tell if his blood pressure med is causing his hallucinations. This system is broken. And yes, I’m mad.
You got this. Start with two visits a week. Ask for the nurse who does the reconciliation. And don’t apologize for asking for help-you’re doing the bravest thing a family can do.
Write a comment