Ever looked in the mirror and noticed dark patches on your face that just won’t go away? You’re not alone. Many people, especially women, deal with uneven skin tone - but not all dark spots are the same. Two of the most common causes are melasma and sun damage. They look similar, but they’re totally different in how they form, how they respond to treatment, and how you need to manage them long-term.
What Exactly Is Hyperpigmentation?
Hyperpigmentation happens when your skin makes too much melanin - the natural pigment that gives skin its color. This overproduction creates darker patches. It’s not dangerous, but it can be frustrating, especially when it shows up on your face where you can’t ignore it. The two biggest culprits? Melasma and solar lentigines (the medical term for sun spots).
Melasma shows up as large, blurry patches - usually on the cheeks, forehead, nose, or upper lip. It’s often symmetrical, meaning both sides of your face look the same. Sun damage, on the other hand, looks like small, well-defined brown spots, often on your hands, shoulders, or décolletage. These aren’t random. They’re direct results of years of sun exposure.
Melasma: More Than Just a Tan
Melasma isn’t caused by the sun alone. That’s the big misunderstanding. Yes, UV light plays a role, but hormones, visible light (like from screens or indoor lighting), and even heat can trigger it. That’s why it’s so common in women during pregnancy, while on birth control, or going through menopause. Studies show that 60-70% of melasma cases in reproductive-age women are tied to hormonal shifts.
It’s also far more common in people with medium to dark skin tones - Black, Asian, and Hispanic populations are 3-5 times more likely to develop it than those with lighter skin. That’s because melanocytes (the cells that make pigment) in these skin types are more active and more easily stimulated.
Here’s the catch: if you treat melasma like a sun spot, you can make it worse. Lasers and intense light therapies that work great for sun damage can actually trigger more pigment in melasma. Why? Because heat and light stimulate the very cells causing the problem. Dermatologists now avoid aggressive treatments until the skin is calm and stable.
Sun Damage: The Slow Burn
Solar lentigines - or sun spots - are simpler. They’re the result of years of UV exposure. Every time your skin gets burned or tanned, melanocytes get overworked and start dumping extra pigment in clusters. By age 60, about 90% of fair-skinned people have them.
Unlike melasma, sun spots respond predictably. A few sessions of IPL (Intense Pulsed Light) or laser treatment can clear them up. Topical treatments like vitamin C or retinoids help too, but lasers are often faster and more effective. The key difference? Sun spots don’t come back if you protect your skin. Melasma? Almost always does.
Topical Treatments: What Actually Works
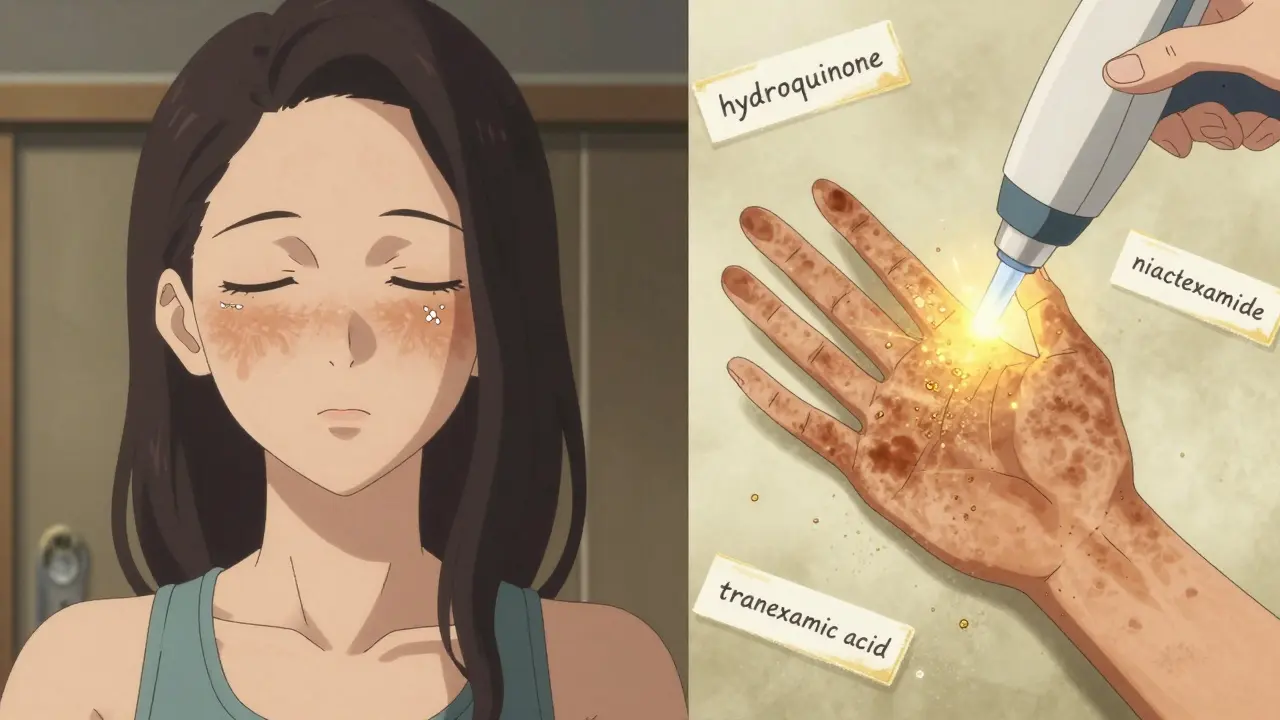
When it comes to creams and serums, not all ingredients are created equal. Here’s what dermatologists actually use:
- Hydroquinone (4%): This is the gold standard. It blocks the enzyme tyrosinase, which your skin needs to make melanin. Used alone, it works for about 50% of people. But when combined with tretinoin and a corticosteroid (a triple therapy), effectiveness jumps to 70%. The catch? You can’t use it longer than 3 months at a time. Long-term use can cause ochronosis - a rare but permanent bluish-black discoloration.
- Tretinoin (0.025-0.1%): A retinoid that speeds up skin cell turnover. It doesn’t lighten pigment directly, but it helps push existing dark spots to the surface so they flake off. It’s usually applied at night, alternating with hydroquinone to reduce irritation.
- Vitamin C (L-ascorbic acid, 10-20%): An antioxidant that reduces existing melanin and blocks new pigment formation. It also fights free radicals from pollution and light. Best applied in the morning under sunscreen.
- Tranexamic acid (5%): Originally a blood-clotting drug, it’s now used topically to calm overactive melanocytes. In clinical trials, it reduced melasma by 45% in 12 weeks with almost no side effects. It’s becoming a go-to for people who can’t tolerate hydroquinone.
- Niacinamide (5%): A gentle, non-irritating option that blocks pigment transfer from melanocytes to skin cells. Great for sensitive skin or as a maintenance product.
Most dermatologists recommend starting with a simple routine: morning - vitamin C + mineral sunscreen; night - tretinoin or tranexamic acid. Add hydroquinone only if needed, and only for short bursts.

The #1 Mistake Everyone Makes
Here’s the truth: no treatment works without sun protection. Not even close.
Most people think SPF 30 is enough. It’s not. For melasma, you need SPF 50+ with iron oxides - yes, the same ingredient in tinted sunscreens. Why? Because visible light (from windows, phones, LEDs) contributes to 25-30% of melasma cases. Regular sunscreens block UV, but not visible light. Iron oxides do.
And don’t just slap it on once. You need about 1/4 teaspoon for your face - that’s the amount that fits on two fingers - and you need to reapply every two hours if you’re outside. Most people use less than half that amount. That’s why 70% of melasma patients see no improvement: they think they’re protected, but they’re not.
Why Lasers Often Fail for Melasma
Laser treatments like IPL or Q-switched lasers are popular. But for melasma? They’re risky. Studies show a 30-40% chance of making the condition worse. Why? Heat. Even a mild laser pulse can trigger melanocytes to go into overdrive.
Dermatologists now use a "melanocyte rest" approach: 8-12 weeks of topical treatment first, to calm the skin. Only then, if needed, do they consider light-based therapy. And even then, they use lower energy settings and avoid treating the entire face.
Sun damage? Totally different. IPL can clear sun spots in one or two sessions. The spots darken, then flake off in a few days. No risk of rebound.
What About Over-the-Counter Products?
Eighty-five percent of people with melasma try OTC products first - whitening creams, brightening serums, natural remedies like lemon juice or licorice root. Most of these don’t contain enough active ingredients to make a real difference.
Some ingredients like kojic acid or azelaic acid can help a little, but they’re not strong enough for stubborn cases. And many OTC products contain hidden steroids or mercury - dangerous and illegal. Stick to brands with transparent labeling and clinical backing.
Long-Term Reality: It’s a Management Game
Melasma isn’t cured. It’s managed. Studies show 95% of people see it return within six months of stopping treatment. That’s why maintenance is non-negotiable.
A good routine includes:
- Morning: Vitamin C serum + mineral sunscreen with iron oxides
- Night: Alternating tretinoin and tranexamic acid (or hydroquinone if tolerated)
- Every 4-6 weeks: Gentle chemical peel (like glycolic or lactic acid) - only if your skin is stable
- Every day: Sunscreen, even if you’re indoors. UV and visible light penetrate windows.
Don’t expect miracles in a week. It takes 8-12 weeks to see improvement. And patience is everything.
What’s Next? The Future of Treatment
Researchers are exploring new options. Cysteamine cream (10%) showed 60% improvement in melasma with minimal irritation in recent trials. Tranexamic acid pills (oral) are also being studied, though topical use is still the safest bet.
And in the future? Dermatologists believe genetic testing may one day tell us which treatment will work best for your specific skin type. For now, the best approach is personalized: match your treatment to your skin tone, triggers, and lifestyle.
Final Takeaway
Melasma and sun damage look alike, but they’re not the same. Melasma needs gentle, consistent care - no lasers, no shortcuts. Sun damage responds quickly to light therapy and strong topicals. But both need the same thing: daily, rigorous sun protection. If you’re serious about clearing dark spots, start with sunscreen. Not tomorrow. Today. Everything else follows from there.
Can melasma go away on its own?
Yes, sometimes - especially if it’s triggered by pregnancy or birth control. After delivery or stopping the pill, melasma can fade over several months. But for most people, especially those with ongoing hormonal or sun exposure triggers, it won’t disappear without treatment. Waiting rarely works.
Is hydroquinone safe?
When used correctly - under a doctor’s guidance, for 3 months at a time, with breaks - hydroquinone is safe for most people. The risk of ochronosis (skin darkening) is low (2-5%) and mostly linked to long-term, unmonitored use. Avoid OTC products with unknown concentrations. In the EU and Japan, it’s banned without a prescription for safety reasons.
Why do I need sunscreen indoors?
Visible light from windows, lamps, and screens can penetrate glass and trigger melasma. Studies show up to 30% of melasma cases are worsened by indoor light exposure. That’s why dermatologists recommend daily sunscreen even if you’re working from home. Mineral sunscreens with iron oxides are best - they block visible light, not just UV.
Can I use retinoids if I have sensitive skin?
Yes, but start slow. Use tretinoin 0.025% every third night for the first month, then gradually increase. Apply a thin layer of moisturizer before it to buffer irritation. If you get redness, peeling, or burning, pause for a few days. Niacinamide or azelaic acid are gentler alternatives that still help lighten pigment.
How long before I see results?
Most people notice improvement in 8-12 weeks with consistent treatment. Full results take 4-6 months. Melasma responds slower than sun damage. If you don’t see change after 3 months, your regimen may need adjustment - talk to a dermatologist. Don’t switch products too often; consistency matters more than intensity.
