JAK Inhibitor Risk Assessment Tool
This tool calculates your relative risk for infections and blood clots based on your personal health factors. The results are estimates based on clinical data, and should be discussed with your doctor.
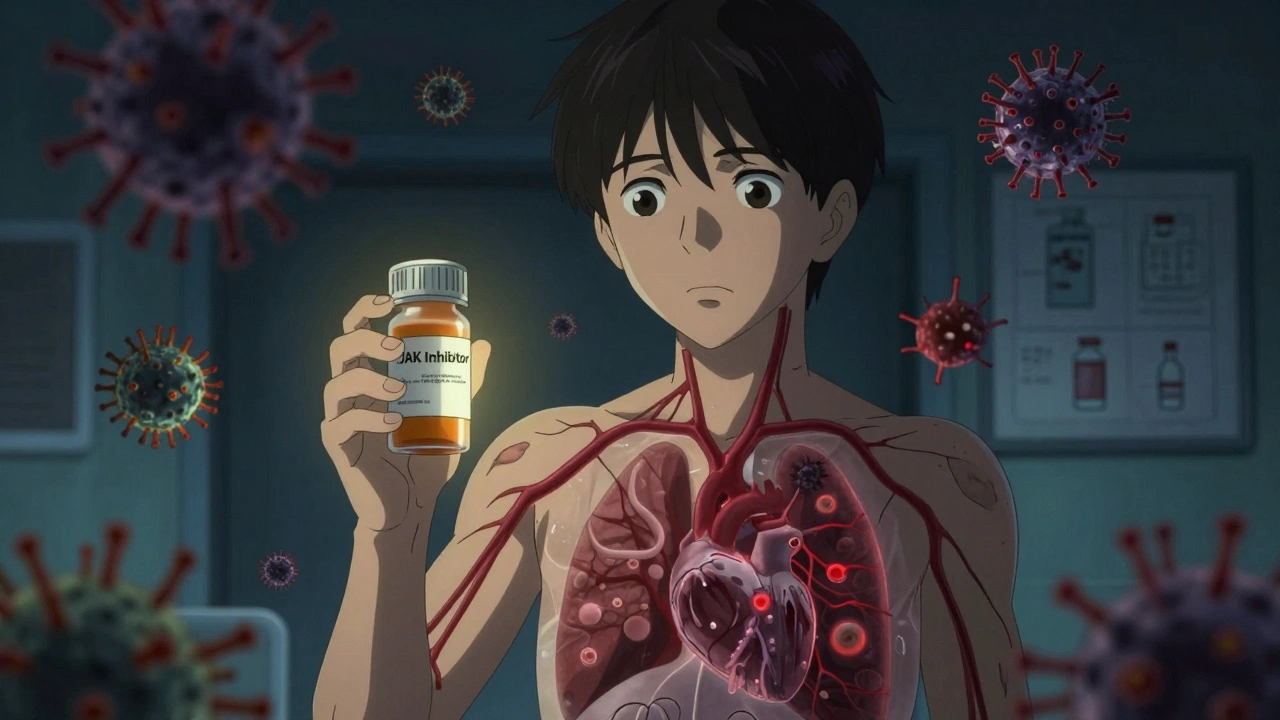
What You Need to Know About JAK Inhibitors and Their Real Risks
When you’re living with rheumatoid arthritis, psoriatic arthritis, or another autoimmune condition, finding a treatment that actually works can feel like a win. JAK inhibitors - drugs like tofacitinib, upadacitinib, and baricitinib - deliver strong results for many people. But behind the relief from joint pain and skin flare-ups is a hidden danger: JAK inhibitors can raise your risk of serious infections and life-threatening blood clots. This isn’t theoretical. It’s backed by years of data, FDA warnings, and real patient stories. If you’re considering or already taking one of these drugs, you need to know what to watch for - and what to ask your doctor.
Why JAK Inhibitors Work - and Why They Put You at Risk
JAK inhibitors block specific enzymes in your immune system called Janus kinases. These enzymes help send signals that trigger inflammation. By slowing them down, the drugs reduce swelling, pain, and tissue damage. But your immune system doesn’t just fight arthritis - it also keeps infections in check. When you suppress it too much, dangerous bugs can slip through.
What’s more, some JAK inhibitors interfere with blood cell production. JAK2 inhibition, in particular, affects platelets and clotting factors. That’s why, even if you’ve never had a blood clot before, your risk jumps. The FDA added a black box warning in 2021 - the strongest possible alert - after a major study showed patients on tofacitinib had higher rates of heart attacks, strokes, and pulmonary embolisms than those on TNF blockers.
The Infection Risks You Can’t Ignore
One in three serious side effects reported with JAK inhibitors involves infection. The most common? Herpes zoster - also known as shingles. Even if you got the shingles vaccine, you’re not fully protected. One patient on Reddit shared how she developed shingles just three months after starting tofacitinib, ending up hospitalized for five days. That’s not rare.
Other serious infections include:
- Tuberculosis (TB)
- Pneumonia
- COVID-19 (more severe outcomes reported)
- Fungal infections like candidiasis and aspergillosis
These aren’t minor colds. They can lead to sepsis, organ failure, or death. That’s why the Infectious Diseases Society of America says you must be up to date on all vaccines - including pneumococcal, influenza, and hepatitis B - at least four weeks before starting treatment. Live vaccines like MMR or varicella are a hard no while you’re on these drugs.
Thrombosis: The Silent Threat
Blood clots don’t always come with warning signs. A deep vein thrombosis (DVT) in your leg might feel like a muscle cramp. A pulmonary embolism (PE) can feel like sudden shortness of breath or chest pain - often mistaken for anxiety or asthma. But the numbers don’t lie. Studies show JAK inhibitors increase the odds of a blood clot by more than double compared to other treatments.
The risk isn’t equal for everyone. If you’re over 65, have a history of clots, smoke, are obese (BMI 30+), or are on estrogen therapy, your risk spikes. One 2023 analysis found patients with prior clots had over five times the risk of another event on JAK inhibitors. Even if you’re young and healthy, a long flight, surgery, or prolonged bed rest can trigger a clot while you’re on these drugs.
The data shows tofacitinib carries the highest clot risk, while newer agents like upadacitinib appear slightly safer - but not risk-free. The FDA and EMA now warn that all JAK inhibitors carry this danger, no matter the brand or condition being treated.
What Your Doctor Should Check Before Prescribing
Not everyone should take a JAK inhibitor. In 2022, the European Medicines Agency made it clear: these drugs should only be used if other treatments - like TNF inhibitors - haven’t worked or aren’t tolerated. And even then, you must pass a strict risk screen.
Before starting, your doctor should:
- Review your personal and family history of blood clots, heart disease, or cancer
- Check your BMI and smoking status
- Confirm you’ve had all required vaccines
- Order a baseline blood count and lipid panel
- Consider a D-dimer test or leg ultrasound if you’re high-risk
Many rheumatology clinics now use standardized checklists for this. If your doctor skips these steps, push back. This isn’t about being difficult - it’s about survival.
Monitoring After You Start: What to Track
Once you’re on a JAK inhibitor, monitoring doesn’t stop. You’ll need regular blood tests:
- Complete blood count every 4 to 8 weeks - to catch low white cells, red cells, or platelets
- Lipid panel at 4 and 12 weeks - JAK inhibitors raise cholesterol by 15-20% in the first month
- Regular check-ins for fever, cough, skin rashes, or unexplained swelling
Cholesterol spikes don’t always cause symptoms, but they add to your long-term heart risk. That’s why statins are often added if levels stay high after 12 weeks.
If you develop a fever over 100.4°F, persistent cough, or sudden leg swelling, don’t wait. Call your doctor immediately. These could be early signs of infection or a clot. Most guidelines say to stop the JAK inhibitor until the issue is resolved.
Real Patient Experiences - What People Are Saying
Online forums are full of stories that textbooks don’t capture. On r/rheumatoidarthritis, users share:
- "I started upadacitinib for my psoriatic arthritis. At six months, I got a DVT after a 6-hour flight. They gave me blood thinners and took me off the drug. I’m still scared to travel."
- "I had shingles on my face while on tofacitinib. It burned for weeks. My vision was affected. I didn’t know the vaccine wasn’t enough."
- "My dad was on baricitinib. He got pneumonia. They didn’t connect it to the drug until it was too late. He didn’t make it."
These aren’t outliers. The FDA’s adverse event database has over 15,000 reports tied to JAK inhibitors since 2012. Nearly half of negative reviews on Drugs.com mention infection or clotting. Patient satisfaction scores hover around 6.2 out of 10 - not because the drugs don’t work, but because the risks are real and sometimes devastating.
When to Say No - And When to Push Back
JAK inhibitors are powerful tools. For some, they’re the only thing that brings relief. But they’re not first-line anymore. The American College of Rheumatology and European League Against Rheumatism both recommend trying TNF inhibitors or other biologics first. Only if those fail should you consider a JAK inhibitor.
If your doctor suggests jumping straight to a JAK inhibitor because it’s “easier” than injections or infusions, ask why. Is it convenience - or risk avoidance on their part? The economic pressure is real: these drugs are expensive, and labs add cost. But your safety should come before billing codes.
And if you’ve had a clot, cancer, or serious infection in the past? Most guidelines say JAK inhibitors are contraindicated. No exceptions.
The Future: Are Safer JAK Inhibitors Coming?
Not all JAK inhibitors are the same. Upadacitinib and filgotinib are more selective - they target JAK1 more than JAK2, which may reduce clotting risk. Early data from the JAKARTA2 trial suggests upadacitinib has a lower clot rate than tofacitinib in low-risk patients. But these are early signals. Long-term data is still being collected.
The FDA and EMA are requiring 10-year post-marketing studies on all JAK inhibitors. A new European registry called JAK-ART is tracking 10,000 patients specifically for clotting events. And new drugs - like TYK2 inhibitors - are in development, aiming to block inflammation without touching blood cell production.
For now, though, the safest choice is still the one with the least risk: avoid JAK inhibitors if you can. If you need them, use them with eyes wide open.
What to Do Right Now
If you’re on a JAK inhibitor:
- Know your risk factors - age, smoking, BMI, past clots, cancer history
- Get your labs done on time - blood count, lipids
- Call your doctor at the first sign of fever, swelling, or chest pain
- Don’t skip vaccines - they’re your first line of defense
If you’re considering one:
- Ask: "What are my alternatives?"
- Ask: "Have you checked my clotting and infection risk?"
- Ask: "Will you stop this if I get sick?"
These drugs can change your life - but only if you survive the treatment. Knowledge isn’t power here. It’s protection.
Can JAK inhibitors cause shingles even if I got the vaccine?
Yes. The shingles vaccine (Shingrix) reduces but doesn’t eliminate risk in people on JAK inhibitors. Studies show up to 14% of patients on these drugs still develop shingles, even after vaccination. That’s why the CDC and IDSA recommend getting vaccinated at least four weeks before starting treatment - and never getting live vaccines while on them.
How long after stopping a JAK inhibitor does the clot risk go down?
The increased clotting risk drops significantly within 30 to 60 days after stopping the drug, based on pharmacokinetic and clinical data. However, if you’ve already had a clot, your baseline risk remains elevated. Your doctor may recommend continuing blood thinners for several months after stopping, especially if you had a pulmonary embolism or DVT.
Are JAK inhibitors safe for younger patients under 50?
Younger patients without risk factors (no smoking, normal weight, no clot history) have a lower absolute risk - but the relative risk is still doubled compared to non-users. The FDA and EMA don’t set an age cutoff, but guidelines strongly advise caution. For patients under 50 with no other risk factors, JAK inhibitors may still be an option if other treatments fail - but only after full discussion of risks.
Do JAK inhibitors increase cancer risk?
Yes. The ORAL Surveillance trial found a 54% higher risk of cancers (excluding skin cancer) in patients on tofacitinib compared to TNF inhibitors. This includes lymphoma, lung cancer, and others. The risk appears dose- and duration-dependent. While the absolute increase is small (about 1.5% over 4 years), it’s real. Regular skin checks and cancer screenings are recommended.
Can I take JAK inhibitors if I’ve had a blood clot before?
No. Most guidelines, including those from the EMA and ACR, consider a prior history of deep vein thrombosis or pulmonary embolism a contraindication to JAK inhibitors. The risk of recurrence is more than five times higher. If you’ve had a clot, your doctor should explore other treatment options like TNF inhibitors or IL-17 blockers.
How often should I get blood tests while on a JAK inhibitor?
You should have a complete blood count every 4 to 8 weeks, especially in the first 6 months. Lipid panels are needed at 4 and 12 weeks after starting, then annually if stable. These tests catch low white cells (infection risk), low platelets (clotting risk), and rising cholesterol - all early warning signs. Skipping them puts you at serious risk.
9 Comments
I got the shingles shot and still got it on tofacitinib. Worst month of my life.
I swear, if one more doctor tells me 'it's just a pill' after I lost my cousin to JAK-related pneumonia... I'm going to scream. They act like we're choosing between coffee and tea. This isn't a lifestyle tweak. It's a gamble with your life. And don't get me started on how they dismiss your fears like you're being dramatic. I'm not dramatic. I'm dead. My cousin is dead. And now I'm stuck on this drug because nothing else works. And yes, I'm still terrified to leave the house.
I'm on upadacitinib and honestly? It's been a game changer for my skin. But I'm on high alert. Got my bloodwork every 4 weeks, took the shingles vaccine 2 months before starting, and I carry a card in my wallet that says 'on JAK inhibitor - if you see me sick, call my rheum doc immediately.' You're not being paranoid - you're being smart. 💪🩺❤️
The FDA black box warning is a marketing tool disguised as science. Most patients on TNF inhibitors get infections too. The data is cherry-picked. You think your risk is higher because you read it online. The absolute risk increase is under 2%. You're more likely to die from a slip in the shower than from a clot on this drug. Stop hyperventilating.
While I appreciate the comprehensive nature of this post, I must emphasize that the statistical interpretation of the ORAL Surveillance trial remains contested in peer-reviewed literature. The hazard ratio for malignancy, while statistically significant, does not translate to clinical significance in low-risk cohorts. Furthermore, the exclusion criteria for the JAKARTA2 trial limit generalizability. One must contextualize risk within individualized pharmacogenomic profiles - not anecdotal Reddit narratives.
i just started upadacitinib last month and honestly i'm scared all the time. i check my legs every night for swelling. i freak out if i get a tiny fever. i know i should be getting bloodwork but i keep putting it off because it feels like waiting for bad news. i just wanted to feel better... why does it have to be this hard?
I’ve been on baricitinib for 18 months. My RA is under control. I’ve had zero infections. I got all my vaccines. I get bloodwork every 6 weeks. I don’t smoke. I’m 42. I’m not obese. I’m not a statistic. This drug saved my life. But I also know it’s not for everyone. Listen to your body. Know your numbers. Don’t let fear silence you - but don’t let convenience blind you either.
You all need to stop being so emotional. If you’re too scared to take a drug that works, don’t take it. But don’t scare people who are doing fine. You think your shingles story is unique? I’ve had 3 bouts of shingles since I was 22 - none of them on JAK inhibitors. You’re conflating correlation with causation. Also, why are you all so obsessed with blood clots? It’s not like you’re not going to die of something. Maybe just… live your life?
Your comment about 'just living your life' is dangerously irresponsible. You're minimizing the documented mortality data. The FDA’s own adverse event database shows 1,200+ deaths linked to JAK inhibitors since 2019 - many from undiagnosed infections or clots. Your anecdote doesn't negate population-level risk. And your tone? Classic gaslighting. People aren't being 'emotional' - they're being survivors. You're not helping. You're endangering.
Write a comment