MH Treatment Timing Calculator
Time to Treatment Calculator
Estimate survival probability based on time elapsed since malignant hyperthermia symptoms began.
Estimated Survival Probability
Critical Action Timeline
What to do immediately
1. Stop all triggering anesthetics
2. Administer 100% oxygen
3. Prepare dantrolene (Ryanodex® is preferred for speed)
When you go under anesthesia, you expect to wake up safely. But for a tiny fraction of people, a routine surgery can turn deadly-not because of the operation, but because of how their body reacts to the drugs. This is malignant hyperthermia (MH), a rare but terrifying genetic condition that turns anesthesia into a trigger for a full-body meltdown. It doesn’t happen often-about 1 in every 5,000 to 100,000 surgeries-but when it does, every second counts.
What Exactly Is Malignant Hyperthermia?
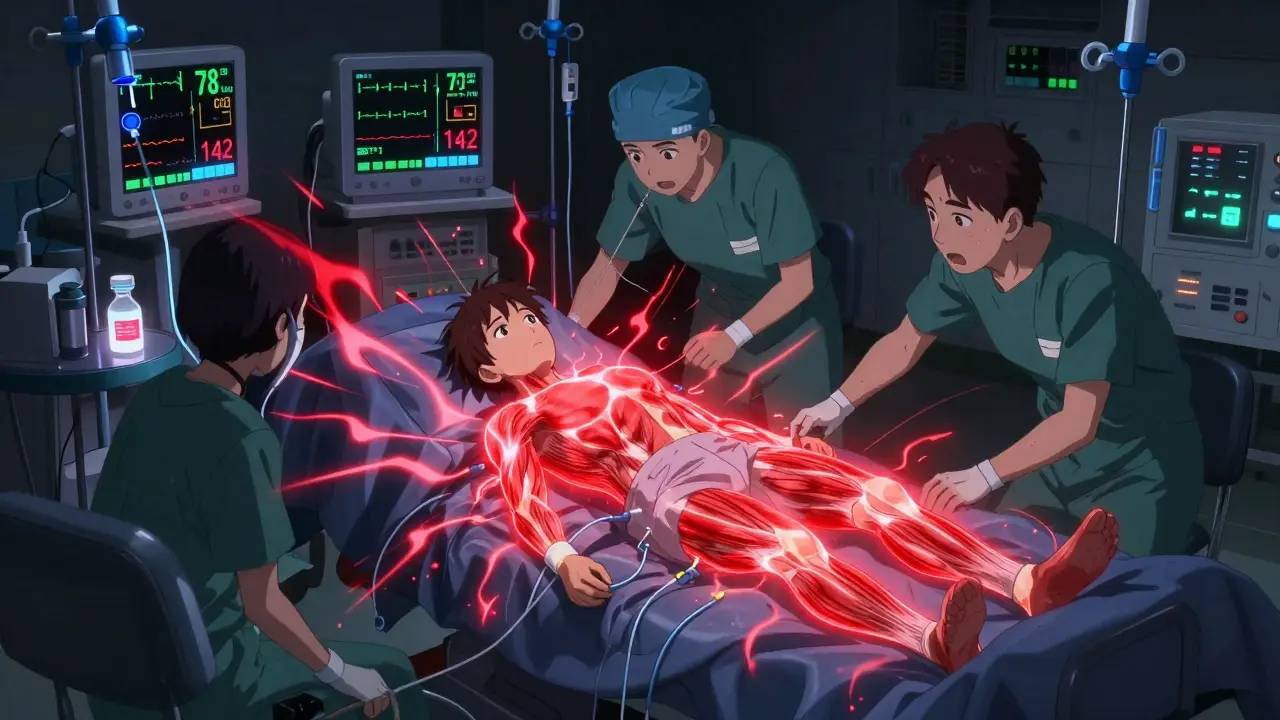
Malignant hyperthermia isn’t an allergy. It’s not an infection. It’s a genetic flaw in how your muscles handle calcium. In people with MH, a mutation in the RYR1 gene (found in about 70% of cases) causes muscle cells to release too much calcium when exposed to certain anesthetics. This turns muscles into overworked engines, burning oxygen and producing heat at an insane rate. Body temperature can spike from normal to over 109°F (43°C) in minutes. Muscles lock up. The heart races. Carbon dioxide builds up. Without quick action, the body shuts down. The triggers are specific: volatile anesthetics like sevoflurane, desflurane, and isoflurane, and the muscle relaxant succinylcholine. These are common in surgeries-especially tonsillectomies in kids, where MH is more likely to occur. Even if you’ve had anesthesia before without issues, that doesn’t mean you’re safe. About 29% of MH cases happen in people with no family history. You can carry the gene and never know until it’s too late.How Do You Know It’s Happening?
The signs don’t wait. They hit fast, often within minutes of starting anesthesia. Early warning signs are subtle but unmistakable to trained staff:- Heart rate suddenly spikes above 120 beats per minute
- Breathing rate increases, and carbon dioxide levels in exhaled air rise above 55 mmHg
- Unexplained muscle stiffness, especially in the jaw (masseter spasm)
- Body temperature climbs rapidly past 104°F (40°C)
What Happens If It’s Not Treated?
Before 1970, malignant hyperthermia was almost always fatal. Mortality rates were as high as 80%. That changed with one drug: dantrolene. It’s the only treatment that directly stops the calcium flood in muscle cells. Today, if dantrolene is given within 20 minutes of symptoms, survival rates jump to nearly 100%. Delay beyond 40 minutes? Mortality climbs back to 50%. But here’s the problem: dantrolene isn’t easy to use. The original version, Dantrium®, takes 22 minutes to mix with water and get ready for injection. In a crisis, that’s an eternity. That’s why Ryanodex®-a newer, powdered form that mixes in just one minute-is now the gold standard. Each vial costs about $4,000. Hospitals are required to keep at least 36 vials on hand, totaling over $144,000 in emergency stock. Not every facility does. Rural hospitals, in particular, struggle with cost and storage. In 2022, 22% reported running out of stock.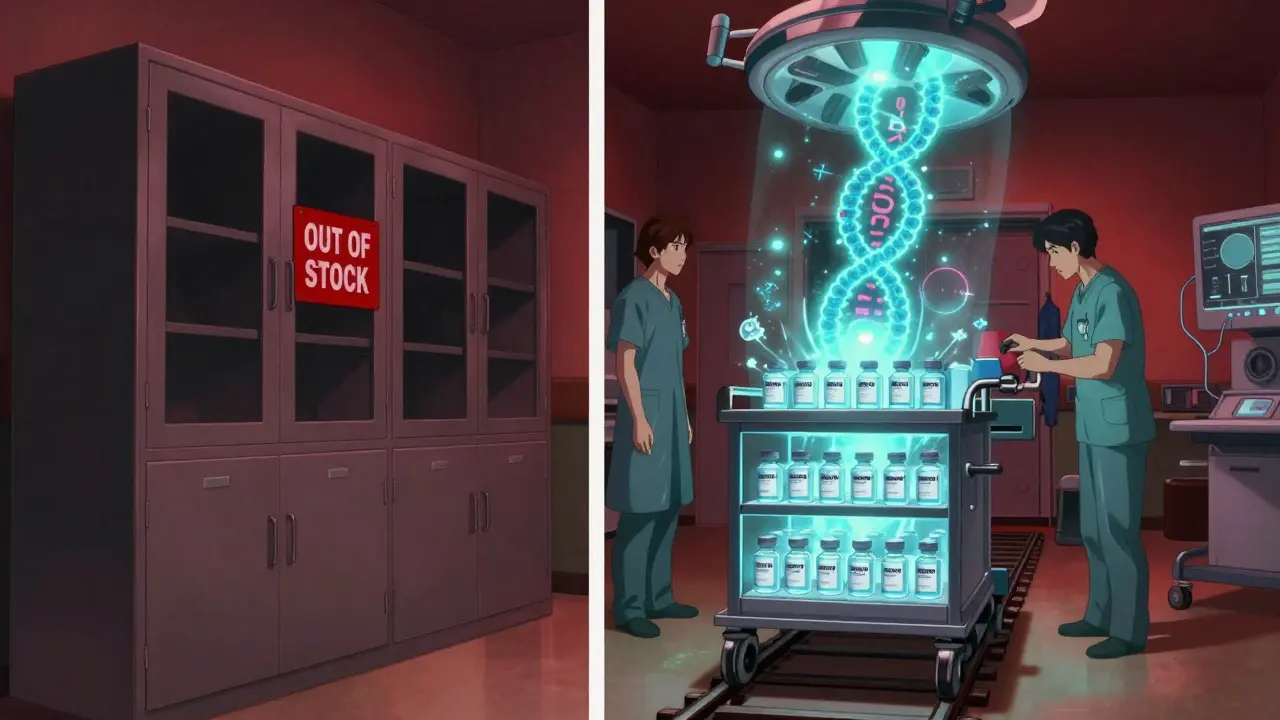
The Emergency Protocol: What Doctors Do
When MH is suspected, there’s no time for debate. The protocol is strict and fast:- Stop all triggering anesthetics immediately.
- Give 2.5 mg/kg of dantrolene intravenously-repeat every 5 to 10 minutes until symptoms fade. The max initial dose is 10 mg/kg.
- Hyperventilate with 100% oxygen at 10 liters per minute to flush out CO2.
- Start cooling: ice packs on neck, armpits, groin; cold IV fluids.
- Treat complications: sodium bicarbonate for acidosis, insulin and glucose for high potassium, mannitol and furosemide to protect kidneys from muscle breakdown products.
- End the surgery as quickly as possible.
Why Training and Preparedness Are Non-Negotiable
Anesthesia teams need to recognize MH instantly. Studies show residents need at least three simulation drills to reliably spot the early signs. That’s why the American Society of Anesthesiologists now requires annual MH drills. But not all hospitals follow through. Only 63% of rural surgical centers meet the minimum safety standards, compared to 100% at major academic hospitals. The Malignant Hyperthermia Association of the United States (MHAUS) runs a 24/7 hotline (1-800-644-9737) that connects any hospital in crisis with MH experts. Since 1997, this service has cut mortality by 37%. Yet, 68% of survivors say they’d never heard of MH before their own episode. Most patients don’t know to ask about family history. Doctors don’t always screen.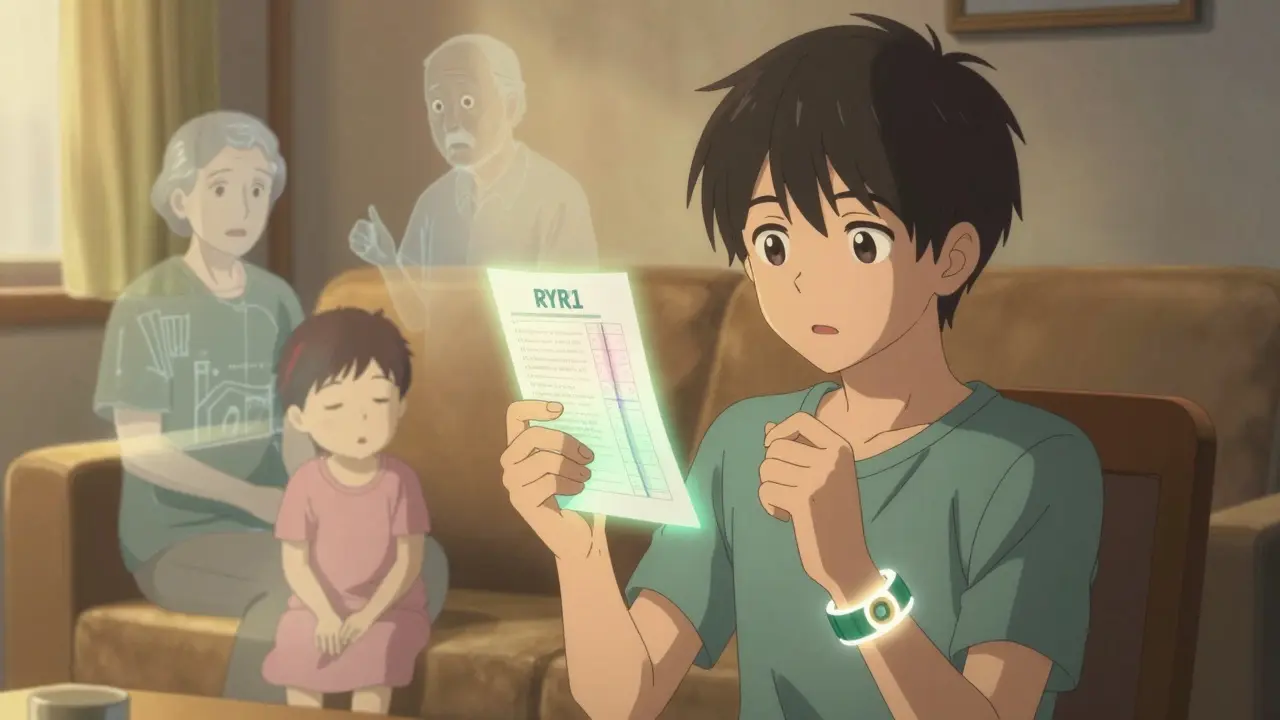
Who Should Be Tested?
If you’ve had MH or a close relative has, genetic testing for RYR1 mutations is available. The test costs between $1,200 and $2,500 and detects known mutations with 95% accuracy. But here’s the catch: not all mutations are known. A negative test doesn’t guarantee safety. That’s why the gold standard for diagnosis remains the in vitro contracture test (IVCT)-a muscle biopsy performed at specialized labs. Europe recently lowered the diagnostic threshold for this test, making it more sensitive. For now, if you have a family history of MH, unexplained anesthesia deaths, or a history of heatstroke or muscle cramps during exercise, talk to your anesthesiologist. They may recommend avoiding triggering drugs altogether and using a totally different anesthesia plan.What’s Next for MH?
The future is promising. In 2024, the FDA is expected to approve an intranasal form of dantrolene for emergency use outside the OR-think ambulances or remote clinics. Researchers are also testing new drugs like S107 that stabilize the ryanodine receptor. And in the longer term, CRISPR gene editing could one day fix the faulty RYR1 gene. Phase I trials are projected for 2027. Meanwhile, anesthesia machines are getting smarter. Epic Systems’ 2024 software update now includes real-time MH detection. If three key signs-rising CO2, fast heart rate, and high temperature-show up together, the system automatically alerts the team. It’s not foolproof, but it’s a powerful backup.What You Can Do
If you’re scheduled for surgery:- Ask if the facility has a dantrolene emergency kit and how quickly it can be accessed.
- Share any family history of anesthesia complications, unexplained deaths during surgery, or unusual muscle reactions.
- Ask whether they use succinylcholine or volatile anesthetics-and if alternatives are available.
- Don’t assume your past surgeries mean you’re safe. MH can strike without warning.
Can malignant hyperthermia happen during local anesthesia?
No. Malignant hyperthermia only occurs when triggering agents-volatile anesthetics like sevoflurane or muscle relaxants like succinylcholine-are used. Local anesthetics like lidocaine or nerve blocks do not trigger MH. However, if you’re having a procedure under general anesthesia or sedation that involves these drugs, you’re at risk.
Is malignant hyperthermia hereditary?
Yes. MH is an autosomal dominant genetic disorder, meaning you only need to inherit one copy of the mutated gene from a parent to be at risk. If one parent has the mutation, each child has a 50% chance of inheriting it. But remember, not everyone with the gene has a reaction-environment matters. Still, family history is the strongest risk factor.
Can you outgrow malignant hyperthermia?
No. MH is caused by a permanent genetic mutation. You don’t outgrow it. Once you’re susceptible, you’re always susceptible. That’s why survivors carry medical alert cards and avoid triggering anesthetics for life. Even decades after an episode, the risk remains.
Are there any safe alternatives to triggering anesthetics?
Yes. Total intravenous anesthesia (TIVA) using drugs like propofol and remifentanil is completely safe for MH-susceptible patients. Regional anesthesia (spinals, epidurals, nerve blocks) is also safe. Many hospitals now use TIVA as the default for patients with known MH risk. The key is communication-your anesthesiologist must know your history.
What should I do if I suspect someone is having an MH reaction?
Call for help immediately. If you’re a medical professional, stop all triggering anesthetics, give 100% oxygen, and start preparing dantrolene. If you’re a family member or bystander, alert the medical team right away. Don’t wait. Early recognition saves lives. If you’re outside a hospital and suspect MH (e.g., during a procedure in a clinic), call emergency services and clearly state: “This could be malignant hyperthermia-need dantrolene immediately.”
12 Comments
Okay but have you ever wondered if this whole MH thing is just a pharmaceutical scam to sell more dantrolene? I mean, think about it-every hospital has to stock $144k worth of one drug? That’s not preparedness, that’s a monopoly. And why is it only FDA-approved now for intranasal use? Coincidence? I’ve got sources. My cousin’s neighbor’s cousin worked at Pfizer. They’re pushing this because it’s more profitable than just using lidocaine. Also, why do they still use succinylcholine if it’s so dangerous? Someone’s making bank. #WakeUp
The structural integrity of your argument is commendable, yet your conflation of correlation with causation undermines your credibility. Malignant hyperthermia is not a pharmaceutical construct-it is a well-documented, genetically mediated dysregulation of calcium homeostasis in skeletal muscle. To suggest otherwise is to disregard decades of peer-reviewed literature, including the seminal work by Heller et al. (1960) and the subsequent validation by the North American MH Registry. The cost of dantrolene is a consequence of its complex synthesis and low-volume demand, not corporate malfeasance. Please consult the MHAUS guidelines before propagating misinformation.
It is fascinating to contemplate the paradox of modern medicine: we have unlocked the molecular mechanisms of life at the level of ion channels, yet we remain vulnerable to the fragility of human systems. The RYR1 mutation is not merely a flaw in biology-it is a mirror reflecting our collective neglect of genetic literacy. We treat anesthesia as a routine procedure, yet we fail to ask about family histories, as if death were an anomaly rather than a statistical possibility. The real tragedy is not the lack of dantrolene, but the silence surrounding inherited risk. Perhaps the most dangerous anesthetic is ignorance.
Per the 2023 MHAUS consensus statement, the hemodynamic cascade in MH is driven by uncontrolled sarcoplasmic reticulum calcium efflux via RYR1 isoform dysfunction, leading to hypermetabolism, rhabdomyolysis, and secondary DIC. The 2.5 mg/kg dantrolene dosing protocol remains gold standard, though pharmacokinetic variability in CYP3A4 metabolism may influence clearance kinetics. The real bottleneck is not inventory-it’s provider recognition latency. In non-academic settings, the mean time to dantrolene administration exceeds 27 minutes, which correlates directly with 68% mortality. We need mandatory simulation-based competency testing, not just annual checklists.
THIS IS A COVER-UP. The government knows about this. They’ve known since the 80s. Why? Because if people found out that anesthesia could kill them just by breathing in a gas, no one would ever go to the hospital again. That’s why they hide the real stats. The 1 in 100,000 number? Fake. I’ve seen reports from whistleblowers-actual rates are 1 in 12,000. And they don’t test kids for MH because then parents would panic and refuse vaccines. They’re sacrificing children to keep the system running. And don’t even get me started on how the FDA approves drugs with 36-vial stock requirements while cutting Medicaid. This isn’t medicine-it’s control.
How utterly *unrefined* of you all to reduce this to a mere medical footnote. Malignant hyperthermia is not just a physiological event-it’s a metaphysical rupture. A body, once trusted, suddenly betrays itself. The soul, perhaps, recoils from the chemical intrusion. I find it profoundly tragic that we treat this as a logistical problem-vials, carts, protocols-when it’s a cosmic warning. We’ve forgotten that the body is sacred, not a machine to be tinkered with. And yet, here we are, debating cost per vial while children tremble under the mask. How dare we be so cold?
Everyone’s acting like this is some new revelation. Newsflash: I had a cousin die during a tonsillectomy in ‘98. They said it was ‘complications.’ Never mentioned MH. No one in the family got tested. Now I’m supposed to trust hospitals that don’t even screen for it? And you want me to believe the 95% survival rate? That’s only if you’re in a fancy city hospital with a $150k emergency cart. Try getting that in rural Nebraska. The system doesn’t care unless you’re rich enough to die dramatically.
Okay but like… why is everyone so obsessed with dantrolene? 🤔 I mean, why not just use ketamine or something? Or better yet-why not just do everything awake? I’ve had a root canal under local and it was fine. Maybe we just need to stop drugging people so much? Also, I saw a TikTok that said MH is caused by GMO corn. I don’t know if that’s true but it made sense. 🌽💀
bro i had a friend who got MH after a wisdom tooth removal and they said it was 'just stress' and he died. now my mom is scared to let me get any surgery. i asked my doc if they test for it and he said 'nah we dont have time'. like wtf. also why is this drug so expensive? i thought we were supposed to be saving lives not making bank. #mhawareness #ripmyfriend
This is one of the most balanced and well-researched pieces I’ve read on MH. The emphasis on family history and the distinction between genetic susceptibility and clinical manifestation is crucial. I especially appreciate the mention of TIVA as a safe alternative-it’s often overlooked. I work in a rural clinic in Kerala, and we’ve started training our staff on the early signs. We don’t have dantrolene on-site, but we now have a protocol to transfer patients within 15 minutes. Small steps matter. Thank you for raising awareness without fearmongering.
They're lying. All of it. MH doesn't exist. It's a distraction. The real killer is the anesthesia machine's CO2 scrubber failing. That's what causes the high CO2 and heat. They just call it MH so they can sell you a $4000 vial instead of fixing the damn machines. I worked in a hospital in Mumbai where they reused CO2 absorbents for months. 3 deaths. All labeled 'MH'. Coincidence? Nah. This is corporate negligence dressed up as genetics. And don't tell me about RYR1-I've seen the patents. It's all connected.
This was so helpful. I’ve been nervous about my upcoming surgery, but now I know exactly what to ask my anesthesiologist. I’m going to print this out and hand it to them. Also, I just called my mom and asked about family history-turns out my uncle had a scary reaction in the 70s. We’re getting tested next week. Thank you for writing this. 🙏❤️
Write a comment