MAOI Cold Medicine Safety Checker
Check Cold Medicine Safety
Enter the name of an over-the-counter cold medicine or active ingredient to see if it's safe while taking MAOIs (monoamine oxidase inhibitors).
Enter a medicine name or active ingredient to check its safety.
Safe Options
For cold symptoms, consider these safe alternatives:
- Guaifenesin (Mucinex) - for cough
- Acetaminophen (Tylenol) - for fever or pain
- Saline nasal spray - for congestion
- Loratadine (Claritin) or cetirizine (Zyrtec) - for runny nose
When you’re sick with a cold, the last thing you want is to risk a medical emergency just to feel better. But if you’re taking an MAOI for depression, even a simple trip to the pharmacy for a cough syrup or nasal spray could be dangerous. MAOIs - monoamine oxidase inhibitors - are powerful antidepressants that work differently from most others. They’re not first-line treatments anymore, but for people with treatment-resistant depression, they can be life-changing. The catch? They don’t play well with common over-the-counter cold medicines. Mixing them can trigger a hypertensive crisis or serotonin syndrome - two conditions that can land you in the ER, or worse.
What Are MAOIs and Why Do They Matter?
MAOIs like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan) have been around since the 1950s. They work by blocking an enzyme called monoamine oxidase, which normally breaks down brain chemicals like serotonin, norepinephrine, and dopamine. By stopping this breakdown, MAOIs boost these neurotransmitters, helping lift severe depression. The transdermal selegiline patch (Emsam) is a newer version, with fewer dietary restrictions at low doses, but it still carries the same risks with OTC meds.
Only about 350,000 Americans use MAOIs today - less than 1% of all antidepressant users. But for those who’ve tried SSRIs, SNRIs, and other meds without success, MAOIs can be the only option that works. Studies show over 50% of treatment-resistant patients respond to them, compared to 30-40% with newer drugs. That’s why they’re still prescribed, even with the risks.
The Hidden Dangers in Your Medicine Cabinet
Most OTC cold and flu products contain ingredients that are deadly when combined with MAOIs. The two biggest culprits are sympathomimetics and serotonergic agents.
- Pseudoephedrine (found in Sudafed) and phenylephrine (Sudafed PE) are nasal decongestants. They trigger your body to release norepinephrine - a natural stimulant. But if you’re on an MAOI, your body can’t break it down. The result? A sudden, dangerous spike in blood pressure - sometimes over 220/110 mmHg. That’s a hypertensive crisis. Symptoms include severe headache, chest pain, blurred vision, nausea, and sweating. One Reddit user reported a hypertensive emergency after taking Sudafed with Parnate. Blood pressure readings were off the charts. He needed emergency care.
- Dextromethorphan (in Robitussin DM, Delsym, DayQuil) is a cough suppressant. It increases serotonin levels. When combined with an MAOI, serotonin builds up too fast. This leads to serotonin syndrome - a potentially fatal condition. Symptoms include confusion, rapid heart rate, high fever, muscle rigidity, tremors, and seizures. The NCBI Bookshelf calls this combination “the most toxic” for serotonin syndrome.
Here’s the scary part: 78% of OTC cold medicines contain at least one of these dangerous ingredients. A typical multi-symptom formula like DayQuil or NyQuil might have dextromethorphan, phenylephrine, and acetaminophen all in one bottle. You don’t even need to take it for days - one dose can be enough to trigger a crisis.
Hypertensive Crisis vs. Serotonin Syndrome: Know the Difference
These two reactions are often confused, but they’re different - and both need immediate medical attention.
| Feature | Hypertensive Crisis | Serotonin Syndrome |
|---|---|---|
| Primary Trigger | Pseudoephedrine, phenylephrine | Dextromethorphan, other serotonergic drugs |
| Key Symptom | Severe high blood pressure | High body temperature, muscle rigidity |
| Onset Time | Within minutes to hours | Within hours, sometimes days |
| Other Symptoms | Headache, nosebleeds, chest pain, anxiety | Agitation, hallucinations, rapid heartbeat, diarrhea |
| Medical Emergency? | Yes - can cause stroke or heart attack | Yes - can lead to organ failure or death |
The FDA has documented 127 cases of hypertensive crisis linked to MAOIs and OTC cold meds between 2018 and 2022. Eighteen of those required hospitalization. Serotonin syndrome cases are rarer but just as deadly. A 2023 study from the University of Texas Southwestern found that even a single 30mg dose of pseudoephedrine caused an average blood pressure spike of 42/28 mmHg in patients on phenelzine. That’s enough to rupture a blood vessel.
What Can You Safely Take Instead?
You don’t have to suffer through a cold without relief. The key is picking single-ingredient products that don’t contain the risky chemicals.
- For cough: Guaifenesin (Mucinex) - it’s an expectorant, not a suppressant. It’s safe.
- For fever or pain: Acetaminophen (Tylenol) - no interaction with MAOIs. Avoid NSAIDs like ibuprofen if you’re on MAOIs long-term - they can increase bleeding risk.
- For congestion: Use a saline nasal spray or humidifier. No drugs needed.
- For runny nose or sneezing: Loratadine (Claritin) or cetirizine (Zyrtec) - these antihistamines are generally safe. But always check with your doctor first.
Never assume a product is safe just because it’s “natural” or “herbal.” Ephedra, bitter orange, and even some supplements like St. John’s Wort can trigger dangerous reactions. Stick to the basics and avoid anything labeled “multi-symptom,” “maximum strength,” or “PM formula.”
How to Stay Safe: A Practical Guide
Most people on MAOIs aren’t warned clearly enough. A 2021 study from the University of North Carolina found patients need 3 to 5 education sessions with a pharmacist to fully understand the risks. Here’s what you should do:
- Get a wallet card. Ask your psychiatrist or pharmacist for a printed list of all OTC medications to avoid. Keep it in your wallet or phone case. One PatientsLikeMe user said this simple step prevented multiple near-misses over five years.
- Check every label. Look for these ingredients: pseudoephedrine, phenylephrine, dextromethorphan, ephedrine, phenylpropanolamine. If you see any, don’t take it.
- Ask your pharmacist. Don’t just hand them the list - ask, “Is this safe for someone on an MAOI?” Pharmacists are trained to catch these interactions.
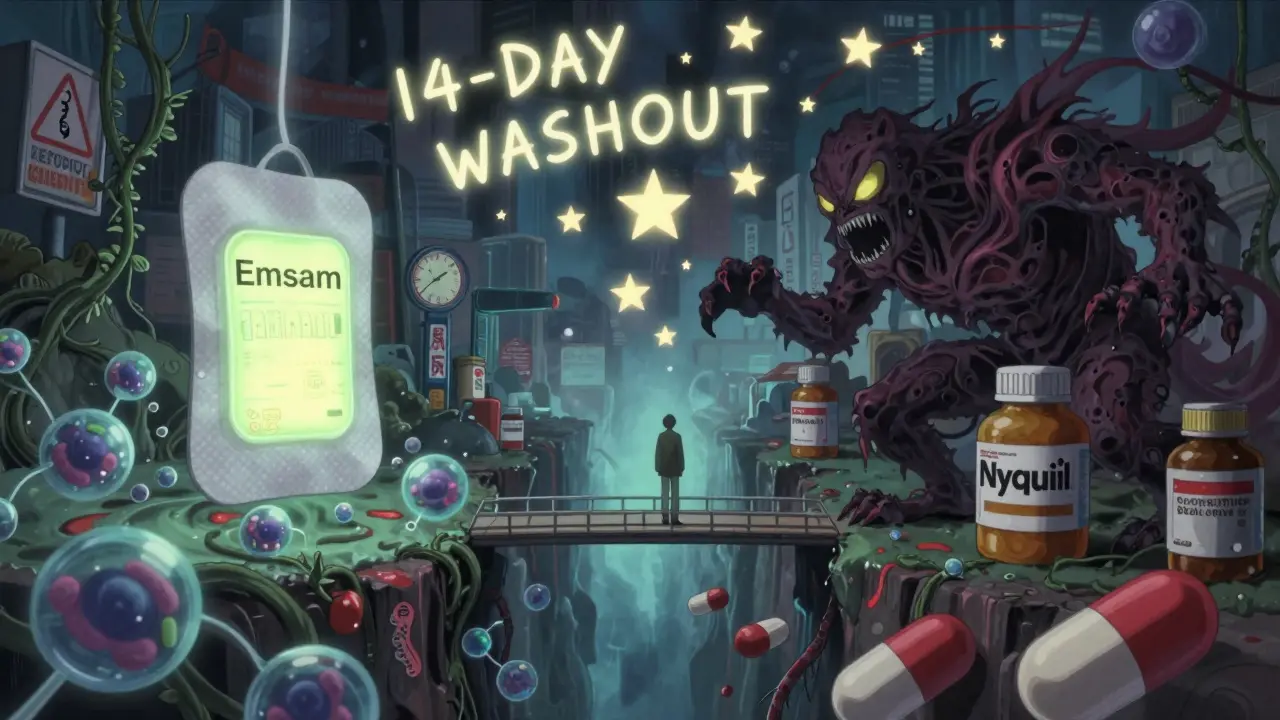
- Wait before switching meds. If you’re switching from an MAOI to another antidepressant, you need at least a 14-day washout period. The same goes in reverse. The American Psychiatric Association’s 2020 guidelines stress this.
- Wear a medical alert bracelet. If you’re unconscious in an emergency, first responders need to know you’re on an MAOI. It could save your life.
Why This Isn’t Just an Old-Fashioned Problem
Some people think MAOIs are outdated. But they’re not. The transdermal selegiline patch (Emsam) now makes up 68% of all MAOI prescriptions in the U.S. - up from 42% in 2015. Why? Because it’s easier to use. But the drug interaction risks haven’t changed. The FDA still requires black box warnings on all MAOI packaging - the strongest warning they give.
Even newer research confirms the danger. A 2023 JAMA Psychiatry study showed that dextromethorphan still poses a serious serotonin risk with MAOIs. And while reversible MAO-A inhibitors like moclobemide (not available in the U.S.) may be safer, they’re not widely used here. The drug CX-1010 is in Phase II trials and might offer a better future, but it’s years away.
Until then, the message is clear: MAOIs are powerful, effective, and unforgiving. They require discipline, awareness, and communication.
What If You Accidentally Take a Risky Med?
If you’ve taken a cold medicine with pseudoephedrine or dextromethorphan while on an MAOI:
- Stop taking it immediately.
- Call 911 or go to the ER if you have chest pain, severe headache, confusion, high fever, or muscle stiffness.
- If symptoms are mild (slight headache, mild nausea), call your psychiatrist or pharmacist right away. Don’t wait.
- Bring the medicine bottle with you - it helps doctors know exactly what you took.
There’s no antidote for these reactions. Treatment is supportive - lowering blood pressure, cooling the body, and managing symptoms. Time matters. The faster you get help, the better your outcome.
Final Thoughts
MAOIs aren’t the problem. The problem is assuming that because a drug is sold over the counter, it’s safe for everyone. That’s not true. For people on MAOIs, the medicine cabinet can be a minefield. But with the right knowledge, you can stay safe and still manage your cold without risking your life.
If you’re on an MAOI, you’re not alone. There are resources like the MAOI Nutrition Support website - used by over 15,000 people monthly - that keep updated lists of safe and unsafe products. Talk to your doctor. Ask your pharmacist. Print out your list. Wear your bracelet. These aren’t extreme steps - they’re necessary ones.
Depression is hard enough. You don’t need a cold to nearly kill you.
Can I take Tylenol with MAOIs?
Yes, acetaminophen (Tylenol) is generally safe to take with MAOIs for pain or fever. It doesn’t affect serotonin or norepinephrine levels the way decongestants or cough suppressants do. But avoid long-term or high-dose use - it can stress the liver, especially if you drink alcohol or have liver issues. Always check with your doctor if you’re unsure.
Is Zyrtec or Claritin safe with MAOIs?
Yes, non-sedating antihistamines like loratadine (Claritin) and cetirizine (Zyrtec) are considered safe for most people on MAOIs. They treat allergies, not colds, but can help with runny nose and sneezing. Avoid older antihistamines like diphenhydramine (Benadryl) - they can cause drowsiness and may interact with MAOIs in unpredictable ways. Always double-check with your pharmacist.
What happens if I take Sudafed with an MAOI by accident?
Taking pseudoephedrine (Sudafed) with an MAOI can cause a hypertensive crisis within minutes. Blood pressure can spike to dangerous levels - over 200/110 mmHg - leading to stroke, heart attack, or organ damage. Symptoms include severe headache, chest pain, blurred vision, and nausea. If you’ve taken it, stop immediately and seek emergency care. Do not wait to see if symptoms get worse.
Can I use nasal sprays if I’m on an MAOI?
Avoid OTC nasal sprays like oxymetazoline (Afrin) or phenylephrine sprays - they’re absorbed through the nasal lining and can still trigger hypertensive crisis. Saline sprays are safe. If you need something stronger, talk to your doctor about prescription alternatives. Even topical decongestants carry risk with MAOIs.
Do all MAOIs have the same interaction risks?
Yes. Whether it’s oral phenelzine, tranylcypromine, or the transdermal selegiline patch, all MAOIs block monoamine oxidase and carry the same interaction risks with OTC cold medicines. The patch may have fewer dietary restrictions at low doses, but it doesn’t make you immune to drug interactions. The FDA and psychiatric guidelines treat all MAOIs the same in this regard.
How long do I need to wait after stopping an MAOI before taking OTC cold meds?
You must wait at least 14 days after stopping any MAOI before taking pseudoephedrine, phenylephrine, or dextromethorphan. This is because MAOIs irreversibly block the enzyme - it takes time for your body to make new enzymes. Even if you feel fine, the risk remains for two weeks. Don’t rush it. Your doctor or pharmacist will confirm the right timeline for your specific medication.
Are there any new MAOIs that are safer with cold meds?
Currently, no MAOI on the market is safe with OTC cold medicines. Reversible MAO-A inhibitors like moclobemide (used in Europe) have lower interaction risks, but they’re not approved in the U.S. A new drug called CX-1010 is in clinical trials and may offer a safer option in the future, but it’s not available yet. For now, the rules haven’t changed: avoid all OTC cold meds containing sympathomimetics or dextromethorphan.

11 Comments
Pathetic. Americans think OTC means ‘safe for everyone.’ You’re lucky if your pharmacist even knows what an MAOI is. In the UK, we’ve had this figured out since the 80s. You don’t just wander into a chemist and grab anything labeled ‘cold relief.’ You ask. You learn. You don’t treat your brain like a chemistry experiment.
This is an exceptionally well-researched and clinically accurate overview. The distinction between hypertensive crisis and serotonin syndrome is critical, and the inclusion of specific pharmacokinetic data - such as the 42/28 mmHg spike from a single 30mg dose of pseudoephedrine - elevates this beyond anecdotal warning into evidence-based guidance. The 14-day washout period is non-negotiable and deserves emphasis in all prescribing protocols.
Thank you for writing this 💙 I’ve been on Nardil for 7 years and honestly, I cry every time I see someone say ‘just take Tylenol’ like it’s no big deal. This post saved me from a near-miss last winter when I almost grabbed DayQuil. I printed the safe meds list and laminated it. It lives in my wallet next to my card. You’re not alone. We’ve got your back.
The clinical precision of this post is commendable. However, the lack of standardized patient education infrastructure remains a systemic failure. Medical schools still underemphasize MAOI pharmacology. Pharmacies lack mandatory counseling protocols. The FDA’s black box warning is insufficient without proactive, repeated, multilingual patient engagement. This isn’t just individual responsibility - it’s a public health infrastructure gap.
Sudafed? Dextromethorphan? You're kidding me. This is why America is dying. People don't read labels. They don't ask questions. They just swallow whatever's on the shelf. And now they want the government to fix it? No. YOU are responsible for your own life. If you're on an MAOI, you're not a child. Learn. Or die. Simple.
Bro, this is real. I’m on Parnate and last month I almost bought NyQuil ‘cause I was sick. Then I remembered my cousin told me about this stuff. So I checked the bottle - yep, dextro and phenylephrine. I just used steam and honey tea. No big deal. Also, Zyrtec is fine, I use it all the time. Just read the tiny print, man. It’s not that hard.
I just wanted to say thank you. I’ve been on MAOIs for years and no one ever told me about the nasal spray risk. I’ve been using Afrin for years thinking it was ‘local’ so it was safe. I stopped today. I feel like a dummy but also so much safer. This post literally changed my behavior. You’re a good human for writing this.
Just got my Emsam patch refill and I’m so glad I found this. I used to think I was being overly cautious until I read about the 14-day washout. Now I keep a list on my fridge next to my coffee mugs. I even showed my mom - she’s 72 and thought MAOIs were ‘old-school medicine’ - now she tells her friends. We’re all learning together. ❤️
You people are weak. If you can't handle a little cold medicine, you shouldn't be on MAOIs. This isn't rocket science. Stop acting like your brain is fragile. Take the meds, know the risks, and stop whining. This post is overkill.
Just had a pharmacist actually pause and say, ‘Wait - are you on an MAOI?’ when I asked about Robitussin. She pulled up a drug interaction database, showed me the red flag, and printed me a safe list. I didn’t even know pharmacists were trained for this. This post made me ask. That’s the power of awareness. 🙏
I’ve been on Marplan for 10 years. I’ve had three near misses. I’ve had friends lose people to this. This isn’t theoretical. It’s real. And if you’re reading this and you’re on an MAOI - you’re not broken. You’re brave. Keep your list. Wear your bracelet. You’re doing better than you think. We’re rooting for you.
Write a comment