Heart Failure Medication Titration Guide
Patient Assessment
Beta-Blockers
Target dose: 25mg carvedilol or 10mg bisoprolol daily
Goal: Resting heart rate 50-60 bpm
Important: Do not increase dose if heart rate < 50 bpm or systolic BP < 90 mmHg
MRAs (Spironolactone/Eplerenone)
Target dose: 25mg daily
| Monitoring Frequency | Before Starting | After 3-7 Days | After Stabilization |
|---|---|---|---|
| Kidney Function (eGFR) | Required | Required | Every 3-6 months |
| Potassium (mEq/L) | Required | Required | Every 3-6 months |
Important: High potassium (>5.5 mEq/L) can cause cardiac arrest
SGLT2 Inhibitors
Target dose: 10mg dapagliflozin or 10mg empagliflozin daily
Important: Monitor for symptoms of DKA even with normal glucose
ARNIs
Target dose: 97/103 mg sacubitril-valsartan twice daily
Important: Hold dose if systolic BP < 90 mmHg
When someone is diagnosed with heart failure, the goal isn’t just to manage symptoms - it’s to extend life. And the most effective way to do that? Heart failure medications given at the right dose, with the right monitoring. But here’s the problem: too many patients never get to those target doses. Why? Because the monitoring is complex, and mistakes can be dangerous.
The current standard, called Guideline-Directed Medical Therapy (GDMT), includes four key drugs: ARNIs, beta-blockers, MRAs, and SGLT2 inhibitors. Each one works differently. Each one needs different checks. And each one carries risks if not watched closely - especially in older adults, women, or people with kidney issues.
Why Target Doses Matter More Than Just Taking Pills
It’s not enough to hand someone a prescription and say, ‘Take this daily.’ Heart failure medications only work when they’re titrated - slowly increased - to the dose proven in trials to save lives. For beta-blockers like carvedilol or bisoprolol, that means getting to 25 mg or 10 mg daily. For MRAs like spironolactone, it’s 25 mg daily. But studies show only 30-40% of eligible patients reach these doses. Why? Because doctors are scared.
Scared of low blood pressure. Scared of high potassium. Scared of kidney trouble. And that fear leads to under-treatment. The truth? When patients reach target doses, their risk of dying from heart failure drops by 35%. That’s not a small gain. That’s life or death.
Monitoring Beta-Blockers: It’s Not Just About Heart Rate
Beta-blockers slow the heart. That’s good - it gives the heart time to recover. But if you slow it too much, the patient gets dizzy or tired. Too little, and the heart keeps working too hard.
The goal? Resting heart rate between 50 and 60 beats per minute. To get there, you start low - maybe 1.25 mg of carvedilol twice a day - and double the dose every 1-2 weeks, as long as the patient isn’t dizzy or their blood pressure doesn’t crash. You check blood pressure and heart rate at every visit. If the heart rate stays above 70 despite maximum tolerated beta-blocker, adding ivabradine can help. But here’s the catch: ivabradine isn’t for everyone. If someone has angina, it can increase their risk of heart attacks by 28%. And if they’re over 75, you start at half the dose: 2.5 mg twice daily.
And don’t forget drug interactions. Strong CYP3A4 inhibitors - like some antifungals or antibiotics - can double ivabradine levels. That’s a recipe for a dangerously slow heart rate.
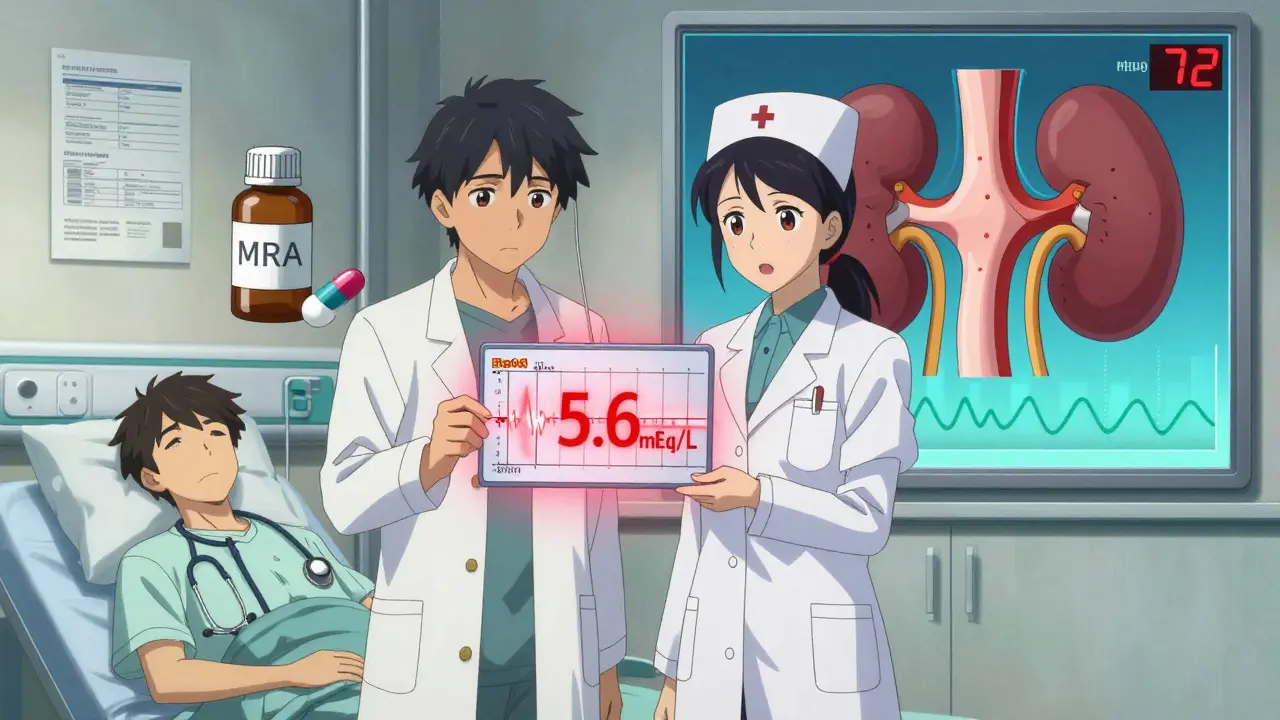
MRAs: The Most Dangerous - and Most Life-Saving - Drug Class
Mineralocorticoid receptor antagonists (MRAs) like spironolactone and eplerenone cut heart failure deaths by 30%. But they also cause hyperkalemia - high potassium - in up to 15% of non-Caucasian patients. That’s nearly twice the rate in white patients. So why do 68% of eligible patients never get this drug? Because labs are skipped.
Here’s the protocol: Check potassium and creatinine before starting. Then again in 3 to 7 days. Then every 3 to 6 months. Skip the first check? You’re gambling with their life. A potassium level over 5.5 mEq/L can cause cardiac arrest. But if you monitor properly, the risk is low. One pilot program that added pharmacist-led checks reduced MRA discontinuations by 42%. That’s not magic - it’s diligence.
Also, watch diuretics. If someone is on furosemide and starts an MRA, they might get dehydrated. Or worse - their kidneys might shut down. You need to balance fluid removal with potassium retention. It’s a tightrope.
SGLT2 Inhibitors: Easier Than You Think - But Still Need Watchful Eyes
SGLT2 inhibitors like dapagliflozin and empagliflozin were originally for diabetes. Now they’re first-line for all types of heart failure - even if the patient doesn’t have diabetes. Why? They cut hospitalizations by 30% and lower death risk. And they’re easier to monitor than MRAs.
But they’re not risk-free. The biggest issue? Genital yeast infections - they happen in 12% of women on these drugs. Men get them too, but less often. Urine tests aren’t needed, but if someone says, ‘It burns when I pee,’ don’t ignore it. Treat it. It’s common. It’s fixable.
Another rare but deadly risk: diabetic ketoacidosis. Even with normal blood sugar. That’s why you check for nausea, vomiting, or deep breathing in anyone who starts this drug. Especially if they’re on insulin or have had recent illness. And in older adults? Watch for volume loss. If they’re on a diuretic and start an SGLT2 inhibitor, they might get too dry. Dehydration can lead to kidney injury.
And here’s the kicker: only 58% of eligible patients are even prescribed these drugs. Why? Because many providers still think they’re only for diabetics. That’s outdated. The 2022 guidelines changed everything. These drugs work for HFpEF, HFmrEF, and HFrEF. If the patient has heart failure - and their kidneys aren’t failing - they should be on one.
ARNIs: The New Powerhouse - But Watch the Blood Pressure
ARNIs like sacubitril-valsartan (Entresto) replaced ACE inhibitors in most cases. They cut heart failure deaths by 20% compared to enalapril. But they cause low blood pressure more often - 14% of patients had symptoms like dizziness or fainting in trials.
That’s why you check blood pressure within 1-2 weeks of starting or increasing the dose. If systolic pressure drops below 90 mm Hg, hold the dose. Don’t panic. Don’t stop forever. Wait a few days, then try again at a lower dose. Some patients need to stay at half the target dose - and that’s okay. Better than hospitalization.
Also, women have 30% higher drug exposure than men. That means more side effects. Start low. Go slow. Especially if they’re older or have low body weight.
Special Populations: One Size Doesn’t Fit All
Heart failure isn’t the same for everyone. Monitoring must change with the patient.
- Older adults (75+): Lower doses of ivabradine. More frequent kidney checks. Watch for falls from dizziness.
- Non-Caucasian patients: Higher risk of hyperkalemia with MRAs. Monitor potassium every 3 days initially.
- Women: Higher drug levels with ARNIs. More genital infections with SGLT2 inhibitors. Don’t assume they’re less at risk.
- People with kidney disease: Avoid MRAs if creatinine is over 2.5 mg/dL or potassium over 5.0 mEq/L. SGLT2 inhibitors are safer here - they protect kidneys.
And forget ‘pill counting.’ Just because someone has 30 pills left doesn’t mean they’re on the right dose. A 2023 study found that 60% of patients who had ‘good adherence’ were still on subtherapeutic doses. That’s not adherence - that’s under-treatment.
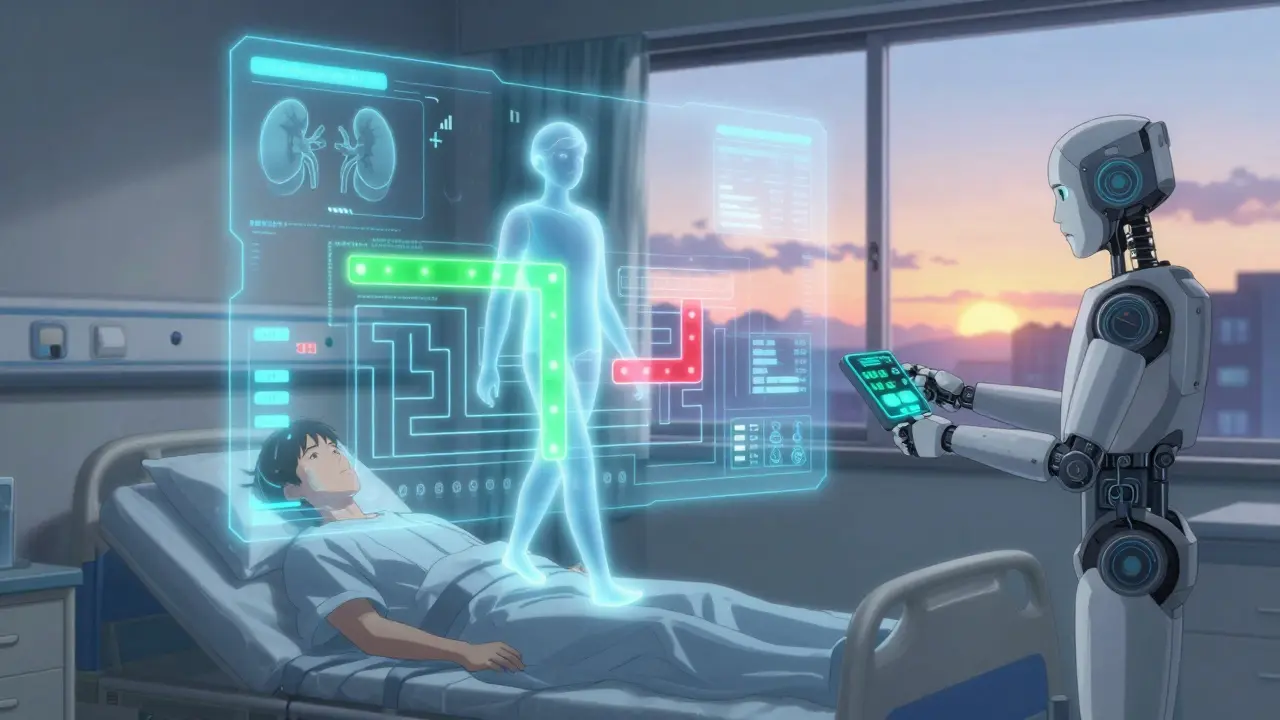
The Future: Smarter Monitoring, Fewer Hospitalizations
The tools are getting better. AI systems now predict hyperkalemia with 83% accuracy by analyzing lab results, medications, and diet. One smartphone app improved medication adherence by 27%. And implantable sensors that track lung pressure can cut hospital visits by 30% - but only 1.2% of eligible patients have them.
Why? Cost. Access. Lack of training. But the future is clear: personalized monitoring. Genetic tests to see who metabolizes drugs slowly. Patches that track potassium in real time. Apps that alert doctors before a patient crashes.
By 2030, 75% of heart failure patients will have custom monitoring plans - based on age, race, kidney function, and genetics. That’s not science fiction. It’s what’s coming.
Right now, we’re stuck in the past. We’re still missing doses. We’re skipping labs. We’re letting fear stop us from giving the best treatment. But it doesn’t have to be this way. With better protocols, better tools, and better training - we can get every patient to target doses. And save more lives.
Why do some heart failure patients never get MRAs even though they’re recommended?
Many doctors avoid MRAs because of fear of high potassium (hyperkalemia), especially in patients with kidney disease or those on other medications that raise potassium. But studies show that with proper monitoring - checking potassium before starting and again within 3-7 days - the risk is manageable. In fact, MRAs reduce death by 30% in heart failure. A 2023 study found that 68% of eligible patients never received an MRA, mostly due to lack of lab follow-up, not actual safety concerns.
Can SGLT2 inhibitors be used in heart failure patients without diabetes?
Yes. Since 2022, guidelines have expanded SGLT2 inhibitors to all types of heart failure - including HFpEF and HFmrEF - regardless of diabetes status. Clinical trials showed they reduce hospitalizations and death even in patients with normal blood sugar. In fact, they’re now considered first-line for most heart failure patients unless contraindicated. The drug works by removing sugar and salt through the kidneys, which reduces fluid overload and improves heart function.
What’s the biggest mistake doctors make when titrating beta-blockers?
The biggest mistake is moving too fast or stopping too soon. Beta-blockers take weeks to reach full effect. Many doctors will start a low dose, see a slight drop in blood pressure, and think it’s too risky - so they never increase it. But the goal isn’t to avoid low blood pressure - it’s to get to the dose proven to save lives. A resting heart rate of 50-60 bpm is the target. If the patient feels okay, even with slightly low BP, you should slowly increase the dose. Waiting for perfect numbers means patients never get the benefit.
Is it safe to combine ivabradine with other heart failure drugs?
Ivabradine can be safely combined with beta-blockers, ARNIs, and SGLT2 inhibitors. But it shouldn’t be used with strong CYP3A4 inhibitors like clarithromycin, ketoconazole, or grapefruit juice - these can raise ivabradine levels by 2.5 to 3 times, causing dangerously slow heart rates. Also, avoid it in patients with angina or recent heart attacks, as the SHIFT trial showed a 28% higher risk of ischemic events. Always check for drug interactions before prescribing.
How often should potassium be checked on an MRA?
Check potassium and kidney function before starting the MRA. Then again within 3 to 7 days after starting or increasing the dose. After that, check every 3 to 6 months if stable. If the patient has kidney disease, is on diuretics, or is elderly, check every 2-4 weeks until stable. Many hospital systems now use automated alerts in electronic records to remind providers - this reduces dangerous discontinuations by 35%.
Do remote monitoring devices actually help prevent heart failure hospitalizations?
Some do - but not all. Implantable pulmonary artery pressure monitors (like the CardioMEMS device) reduced hospitalizations by 30% in high-risk patients with prior hospitalizations, as shown in the CHAMPION trial. But the larger GUIDE-HF trial didn’t show benefit for all patients. Real-world use is still low - under 2% of eligible patients have them. Simpler, noninvasive tools like daily weight tracking, blood pressure logs, and symptom apps are more widely available and show promise. The key isn’t the device - it’s consistent data review and timely intervention.
Heart failure treatment has changed dramatically in the last five years. The medications are better. The guidelines are clearer. But the gap between what we know and what we do is still wide. The fix isn’t more drugs - it’s better monitoring. Smarter checks. More follow-up. And never letting fear stop a patient from getting the dose that could save their life.