Rifampin Sleep Risk Calculator
Key Takeaways
- Rifampin can disrupt sleep by altering liver enzymes and circadian rhythms.
- Taking the dose in the morning and practicing good sleep hygiene reduces insomnia.
- Melatonin and timing adjustments are safe for most patients but should be discussed with a clinician.
- Persistent sleep problems or signs of liver trouble merit prompt medical attention.
- Compared with other TB drugs, rifampin has the highest reported rate of sleep‑related side effects.
What Is Rifampin?
Rifampin is a broad‑spectrum antibiotic belonging to the rifamycin class, primarily used to treat tuberculosis (TB) and certain bacterial infections. It works by binding to the bacterial DNA‑dependent RNA polymerase, halting RNA synthesis and effectively killing the microbe. Rifampin was first approved in the early 1970s and today remains a cornerstone of the standard 6‑month TB regimen.
How Rifampin Works and Why It Can Disrupt Sleep
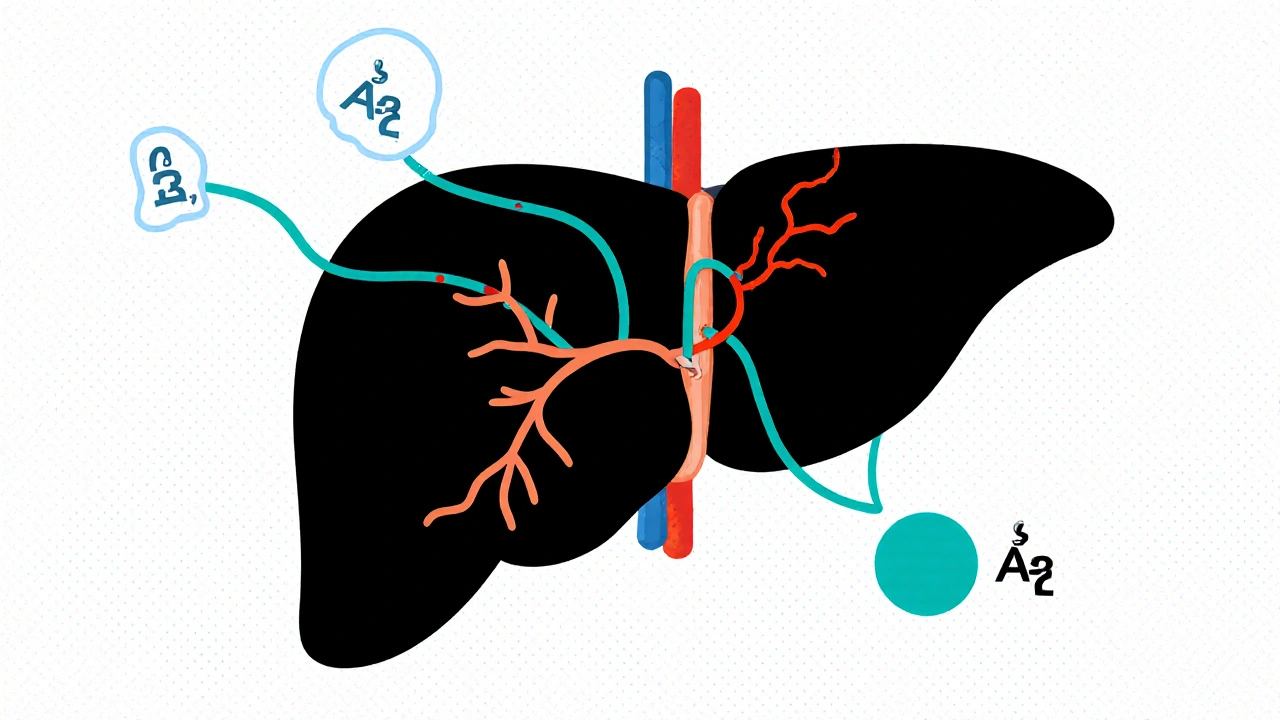
Beyond its antimicrobial action, rifampin is a powerful inducer of the liver’s Cytochrome P450 enzyme system, especially CYP3A4. When these enzymes speed up, they also accelerate the metabolism of endogenous hormones that regulate the sleep‑wake cycle, such as melatonin. Faster melatonin clearance can lead to lower nighttime levels, making it harder to fall asleep.
In addition, rifampin’s influence on bilirubin and other metabolites can cause subtle changes in the brain’s neurotransmitter balance, sometimes resulting in vivid dreams or nighttime restlessness. The net effect is that many patients notice a shift in their usual sleep pattern the first few weeks of therapy.
Common Sleep‑Related Side Effects Reported
Clinical trials and post‑marketing surveys consistently flag the following sleep issues:
- Insomnia - difficulty falling or staying asleep, reported in up to 15% of adults on rifampin.
- Restless legs or muscle twitching, often described as “jumpy” legs just before bedtime.
- Vivid or unsettling dreams, especially when the dose is taken later in the day.
- Early‑morning awakening with an inability to return to sleep.
These symptoms typically emerge within the first two weeks and may improve as the body adjusts, but they can persist for the duration of treatment if not addressed.
Factors That Influence the Sleep Impact
Several variables dictate how strongly rifampin will affect your rest:
- Timing of the dose. Taking rifampin in the evening can amplify nighttime enzyme activity, dropping melatonin when you need it most.
- Liver function. Pre‑existing liver disease reduces the organ’s ability to manage the rapid enzyme turnover, magnifying hormonal swings.
- Concurrent medications. Drugs such as fluconazole, certain antiretrovirals, or even over‑the‑counter sleep aids can either blunt or intensify rifampin’s enzyme‑inducing effect.
- Genetic variations. Polymorphisms in CYP3A4 may make some people “super‑inducers,” experiencing more pronounced insomnia.
Practical Strategies to Improve Sleep While on Rifampin
Below are evidence‑based steps you can take right now:
- Morning dosing. Aim to take rifampin before 10a.m. This aligns peak enzyme activity with daylight, sparing the night‑time melatonin dip.
- Sleep hygiene checklist.
- Dim lights 1hour before bed to signal melatonin production.
- Keep the bedroom cool (18‑20°C) and quiet.
- Limit caffeine after noon and avoid heavy meals after 7p.m.
- Melatonin supplementation. A low dose (0.5mg-1mg) taken 30minutes before bedtime can compensate for the faster clearance caused by rifampin. Discuss dosage with your clinician, especially if you’re on other CYP‑interacting drugs.
- Mind‑body techniques. Progressive muscle relaxation, guided imagery, or short meditation sessions have shown modest benefit for drug‑induced insomnia.
- Avoid other stimulants. Nicotine, alcohol, and certain antihistamines can worsen sleep fragmentation when combined with rifampin’s enzyme induction.

When to Seek Medical Advice
If any of the following occur, contact your healthcare provider promptly:
- Insomnia persisting longer than two weeks despite sleep‑hygiene attempts.
- Excessive daytime fatigue that interferes with work or safety‑critical tasks.
- Yellowing of the skin or eyes, dark urine, or unexplained abdominal pain - possible signs of rifampin‑related liver stress.
- Severe or frightening nightmares that cause anxiety about bedtime.
Your clinician may adjust the dosing schedule, prescribe a short‑term sleep aid, or evaluate liver enzymes to rule out toxicity.
Comparing Rifampin’s Sleep Impact With Other TB Drugs
| Drug | Typical Dosage | Incidence of Insomnia | Other Sleep Issues |
|---|---|---|---|
| Rifampin | 10mg/kg (max 600mg) daily | ≈15% | Vivid dreams, early awakening |
| Isoniazid | 5mg/kg (max 300mg) daily | ≈5% | Peripheral neuropathy can disturb sleep |
| Ethambutol | 15mg/kg (max 1.6g) daily | <1% | Usually none; visual side effects may cause anxiety |
| Pyridoxine (B6 supplement) | 10-50mg daily (given with isoniazid) | 0% | Rarely causes vivid dreams when dosage is high |
Notice that rifampin tops the list for insomnia, making proactive sleep management a priority when it’s part of your regimen.
Frequently Asked Questions
Can I take rifampin at night to avoid daytime side effects?
Night‑time dosing is not recommended because the drug’s enzyme‑inducing effect peaks during sleep, lowering melatonin and increasing insomnia risk. If night dosing is unavoidable, talk to your doctor about a low‑dose melatonin supplement.
Is it safe to use over‑the‑counter sleep aids while on rifampin?
Many OTC antihistamines (e.g., diphenhydramine) are metabolized by CYP3A4 and may become less effective when you’re on rifampin. Consult your prescriber; short‑term prescription‑only hypnotics are often a safer choice.
Does rifampin affect my partner’s sleep?
Rifampin can cause vivid dreams that may lead to talking or moving in sleep, which could disturb a partner. Adjusting the dose timing and keeping the bedroom environment calm can mitigate this.
What lab tests should I monitor while experiencing insomnia on rifampin?
Baseline and periodic liver function tests (ALT, AST, bilirubin) are standard. If insomnia worsens, your doctor might also check serum melatonin or vitamin B6 levels, especially if you’re taking isoniazid concurrently.
Can lifestyle changes alone fix rifampin‑related insomnia?
For many, consistent sleep‑hygiene plus morning dosing resolves the issue. However, a subset needs supplemental melatonin or a brief prescription sleep aid. Always involve your healthcare team before adding supplements.

11 Comments
Rifampin steals your night like a thief in the dark it messes with melatonin and leaves you tossing and turning. The liver enzymes go wild and your body cant keep a steady rhythm. You end up staring at the ceiling while the drug does its work. It feels like a battle between medicine and sleep and most nights you lose.
Dear reader, thank you for sharing this comprehensive overview. It is commendable how thoroughly the mechanisms are explained, especially the role of CYP3A4 induction. I would like to emphasize the importance of maintaining a consistent morning dosing schedule, as this aligns with circadian biology. Additionally, practicing disciplined sleep hygiene can markedly improve outcomes for patients undergoing rifampin therapy.
Great summary! I’ve found that taking my dose before 9 am really helps keep my nights quiet. Also, dimming lights an hour before bed seems to boost melatonin naturally. If you can, avoid caffeine after lunch – it makes the insomnia worse. Keep sharing these tips, they’re super useful.
Thank you for the detailed information. From a clinical perspective, the interaction between rifampin and melatonin metabolism is well documented. Patients should be counseled on the timing of both medication and sleep‑aid supplementation. Monitoring liver function tests periodically is also advisable to preempt potential hepatotoxicity.
First and foremost, let me acknowledge the depth of this article – it truly covers the multifaceted nature of rifampin‑induced sleep disturbances.
It is essential to understand that the enzyme induction caused by rifampin is not merely a biochemical curiosity but a real-world factor that can upend a patient’s nightly routine.
When you consider the half‑life of melatonin and how quickly rifampin accelerates its clearance, the downstream effects become crystal clear.
Consequently, clinicians should prioritize morning dosing to synchronize peak drug activity with daylight, thereby preserving nocturnal melatonin peaks.
In practice, this simple scheduling tweak can reduce insomnia rates dramatically, which is both cost‑effective and patient‑friendly.
Beyond dosing, the article’s sleep‑hygiene checklist is a gold standard; dim lighting, a cool bedroom, and avoidance of caffeine after noon are foundational pillars.
Moreover, incorporating low‑dose melatonin (0.5 to 1 mg) can act as a bridge while the body adjusts, but this must be done under medical supervision to avoid unwanted interactions.
For those with pre‑existing liver conditions, extra vigilance is warranted, as compromised hepatic function can amplify rifampin’s enzyme‑inducing potency.
Genetic polymorphisms in CYP3A4 also play a role, highlighting the need for personalized medicine approaches when feasible.
Patients reporting vivid dreams or early‑morning awakenings should be reassured that these are recognized side effects and often transient.
If symptoms persist beyond two weeks, escalation to short‑term sleep aids may be justified, always balancing benefits against potential dependency risks.
The comparative table underscores that rifampin leads among first‑line TB drugs in sleep‑related adverse events, reinforcing the need for proactive management.
Healthcare providers should maintain an open dialogue about these issues, as patients frequently under‑report sleep problems out of fear of being perceived as non‑compliant.
Ultimately, the goal is to ensure successful TB treatment without sacrificing quality of life, and this article provides a roadmap to achieve that balance.
Thank you for shedding light on such an important, yet often overlooked, aspect of TB therapy.
The pharmacokinetic profile of rifampin is a textbook case of enzyme induction, leading to upregulated CYP3A4 activity and downstream hormonal dysregulation. From a mechanistic standpoint, the accelerated catabolism of endogenous melatonin compromises the circadian feedback loop. Clinicians must therefore adopt a chronopharmacological approach when prescribing. Neglecting this nuance can precipitate iatrogenic insomnia and diminished therapeutic adherence.
I appreciate the thoroughness of the post. It is important to respect patient autonomy while offering evidence‑based recommendations. A balanced approach, encouraging morning dosing and proper sleep hygiene, aligns well with best practices. Please continue to provide such valuable insights.
lol this drug totally ruins sleep haha
One must ponder the very essence of sleep when a molecule like rifampin invades the body's natural rhythm. The harsh truth is that this drug, forged in laboratories, often disregards the humble human need for rest. It is not merely a side effect but a manifestation of how science can sometimes trample on innate biological harmony. We, as a society, should question the complacency that accepts such disruption without protest. Yet, the cure for tuberculosis remains paramount, and we must navigate this paradox with intellect and resolve. Remember, the night belongs to the dreamer, not the pill.
Indeed, the points raised are quite significant, especially regarding the timing of dosage, which, as we all know, can dramatically alter pharmacodynamic outcomes; additionally, the emphasis on sleep hygiene cannot be overstated, because a well‑structured bedtime routine, coupled with reduced exposure to stimulants, can mitigate many of the insomnia complaints that arise from rifampin therapy; finally, patients should be encouraged to monitor their symptoms closely, reporting any persistent disturbances to their healthcare providers without delay.
Nice work! This info helps a lot. I’ll try taking my dose early and keep my room cool. Thanks for the clear tips.
Write a comment