Why Prescription Label Instructions Matter More Than You Think
Every time you pick up a prescription, there’s a small label stuck to the bottle. It says how many pills to take and when. But buried in that text are special instructions-the hidden rules that can mean the difference between your medicine working or causing harm. These aren’t just reminders. They’re safety nets. And if you miss them, you’re at risk.
One in two people misunderstand these instructions. That’s not a small number. That’s millions of people taking pills the wrong way, every single day. Some take antibiotics on an empty stomach when they should’ve eaten first. Others crush pills that were meant to be swallowed whole. A few even ignore the ‘refrigerate’ note and leave life-saving drugs in a warm cabinet. These mistakes aren’t always obvious. But they’re expensive. In the U.S., medication errors tied to unclear labels cost the system over $42 billion a year. And a lot of those errors come down to one thing: not understanding what the special instructions actually mean.
What Counts as a Special Instruction?
Special instructions go beyond ‘take one tablet daily.’ They’re the fine print that changes how your body reacts to the drug. Common ones you’ll see:
- Take with food
- Take on an empty stomach
- Shake well before use
- Refrigerate
- Do not crush or chew
- Avoid sunlight
- Take every 12 hours
- Discard after 14 days
These aren’t suggestions. They’re science-backed rules. For example, taking certain antibiotics without food can cause nausea so severe you stop taking them. Crushing a time-release pill can flood your system with too much medicine at once. Leaving insulin unrefrigerated can make it useless. The FDA requires these instructions because they’ve seen what happens when people guess.
And they’re not all in the same place. About 32% are printed right on the bottle. Nearly half (47%) are on a small sticker stuck on the side. The rest? Hidden in a paper insert you might toss before reading. If you don’t check all three spots, you’re missing critical info.
Why People Keep Getting It Wrong
It’s not that people are careless. It’s that the language is confusing-even for smart, educated folks.
Take ‘take with food.’ What does that mean? A 2021 Harvard study found people interpret it three different ways: 41% think it means ‘with the first bite,’ 33% believe it’s ‘during the meal,’ and 26% think ‘within 30 minutes’ is enough. All three are wrong for different drugs. For some, you need a full meal. For others, a handful of crackers is enough. You won’t know unless you ask.
Timing is another trap. ‘Take every 12 hours’ sounds simple. But 53% of patients take doses too close together-like 8 p.m. and 11 p.m.-because they think ‘every 12 hours’ means ‘twice a day.’ That’s dangerous. It can lead to overdose, especially with painkillers or blood thinners.
And it gets worse for people with low health literacy. About 36% of U.S. adults struggle to read and understand basic health info. For them, the error rate jumps to 62%. Spanish-speaking patients misinterpret ‘take with food’ instructions over three times more often than English speakers. The labels haven’t changed. The problem is the gap between what’s written and what’s understood.
Where to Find the Hidden Instructions
Don’t assume the main label tells you everything. You need to check three places every time you get a new prescription:
- The bottle label-this is the big text you see right away. Look for bold or italicized phrases.
- The sticker-often small, white, and stuck near the cap or on the side. These are used when instructions are added after the bottle was printed.
- The paper insert-the folded sheet that comes with the bottle. Many people throw this away thinking it’s just marketing. But it’s where the FDA requires detailed warnings for high-risk drugs.
Some medications, like blood thinners or chemotherapy drugs, come with a separate Medication Guide. These are required by law for about 250 drugs-roughly 12% of all prescriptions. If your pharmacist hands you a small booklet with a red border, don’t ignore it. It’s not optional. It’s safety documentation.
And here’s a tip: If you see a symbol you don’t recognize-like a sun with a line through it, or a fridge icon-that’s not decoration. The FDA allows these icons, but only 15% of U.S. labels use them. In Europe, over 60% do. That’s why so many people are confused. We’re behind on visual help.
What You Can Do to Stay Safe
Here’s how to protect yourself-no matter your age, education, or language skills:
- Ask the pharmacist to explain it out loud. Don’t just nod. Say, ‘Can you tell me what ‘take with food’ means for this pill?’ They’re trained to break it down. And 89% of positive pharmacy reviews mention this exact help.
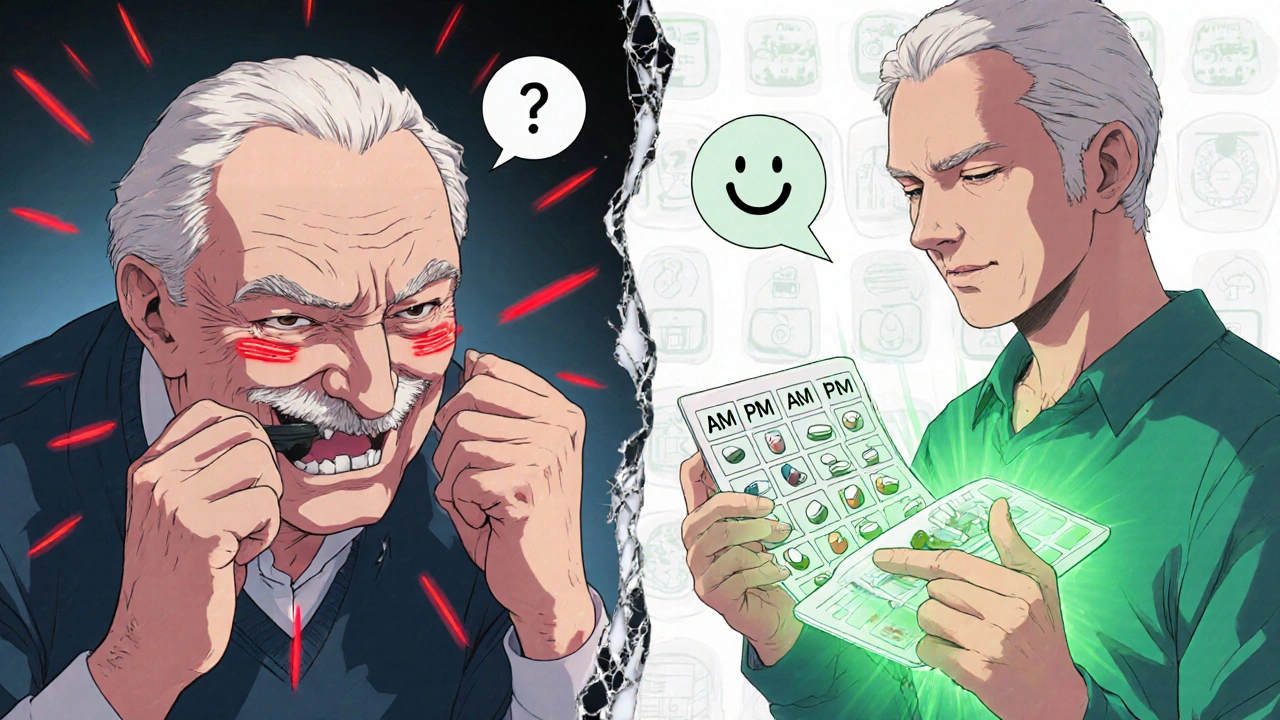
- Use a pill organizer with time slots. If you’re taking pills every 12 hours, a 7-day organizer with AM/PM compartments cuts timing errors by nearly half. Mayo Clinic found this one change alone reduces mistakes.
- Request large-print labels. Over 94% of U.S. pharmacies can print bigger text on request. No extra cost. Just ask.
- Use a reminder app. Apps like Medisafe or MyTherapy let you set alerts for doses and even show you a photo of your pill. Sixty-two percent of users say it helps them stick to instructions.
- Write it down. After your pharmacist explains, jot it on a sticky note. Put it on your mirror or fridge. ‘Take with breakfast. Do not crush.’ Simple. Clear. Visible.
And if you’re caring for an elderly parent or someone with memory issues? Don’t rely on them to remember. Set up a system. Use a weekly pill box. Put the bottle where they’ll see it. Call the pharmacy if something doesn’t make sense.

What’s Changing on the Horizon
Change is coming. The FDA is pushing for standardization. By 2026, they plan to require the same wording for 12 key instructions across all labels. ‘Take with food’ won’t be vague anymore. It’ll be defined: ‘Take with a full meal.’ ‘Take on empty stomach’ will mean ‘at least one hour before or two hours after eating.’
Pharmacies are testing AI tools that adjust label language based on your reading level. If you’ve had trouble understanding labels before, the system might automatically print a simpler version. Some are even testing augmented reality labels-scan the bottle with your phone and watch a 30-second video of how to take the pill.
And now, doctors can bill for a 5-minute session just to explain medication instructions. That’s new. It’s called CPT code 99444. It’s worth $27.63 per visit. That means more providers are being paid to sit down and make sure you understand.
But here’s the hard truth: labels alone won’t fix everything. Dr. David Bates from Harvard says without fixing health literacy across the population, label improvements will only solve 40% of the problem. That’s why your role matters. You’re not just a patient. You’re part of the solution.
When to Call Your Pharmacist
You don’t need to guess. If any of these sound familiar, call your pharmacy right away:
- You’re not sure if you should take the pill with food or not
- You missed a dose and don’t know whether to take it now or skip it
- You’re confused about ‘every 12 hours’ versus ‘twice a day’
- You can’t find the instructions on the bottle or insert
- The label says ‘do not crush’ but the pill is too big to swallow
Pharmacists are your best resource. They see hundreds of prescriptions every day. They know what gets misread. And they’re paid to help you get it right. Don’t wait until you feel sick. Call before you take the first pill.
Final Thought: Your Health Is in the Details
Prescription labels aren’t just paperwork. They’re your protection. The difference between healing and harm often comes down to a single phrase. ‘Take with food.’ ‘Shake well.’ ‘Refrigerate.’
Don’t assume. Don’t guess. Don’t ignore the small print. Ask. Write it down. Use tools. And if something doesn’t make sense-speak up. Your life might depend on it.

11 Comments
i just take my pills when i remember lol who has time to read all that stuff
my grandma died cause she thought 'take with food' meant like...a snack? not a full meal
rip
so basically the pharma industry wants us to be pharmacists but won't pay us for it? genius move.
also why does my bottle say 'shake well' like i'm making a cocktail and not saving my life?
yall ever notice how the only people who actually read the insert are the ones who already know they're gonna mess up?
the rest of us? we glance at the big letters, nod like we got it, then take it with coffee because 'why not'?
the system is broken. not the patient. the system.
also i use medisafe and it saved me from taking my blood thinner at 2am. that thing beeps like a tiny angry robot and i love it
they're hiding the real truth in those labels
the 'do not crush' thing? that's because the pill is actually a tracking chip
they're monitoring your compliance
you think the FDA cares about you? nah
they care about the data
and the fridge icon? that's not for the medicine
it's to keep your phone cool while it uploads your pill-taking habits to the cloud
we're all lab rats now
:(
as a clinical pharmacist, i can tell you the biggest issue isn't the wording-it's cognitive load. patients are juggling 5+ meds, appointments, insurance forms, and family stress. the label is the last thing on their mind.
that's why the 5-minute counseling code (CPT 99444) is a game-changer. it's not about the money-it's about validation. if you're not getting this time, ask for it. you're entitled.
also: pill organizers with alarms? non-negotiable. i've seen lives changed by a $12 plastic box.
in india we dont have all these labels
pharmacist just tells you what to do
and if you dont understand you ask again
no stickers no inserts just talk
maybe we need more talking less paper
The empirical data presented herein underscores a systemic deficiency in patient-healthcare communication infrastructure. The prevalence of misinterpretation of pharmacological directives correlates strongly with socioeconomic determinants of health literacy, as evidenced by the 62% error rate among low-literacy cohorts. It is imperative that pharmaceutical labeling protocols be harmonized with cognitive load theory and universal design principles to mitigate iatrogenic harm.
i used to think these labels were just boring fine print
until my dad almost died because he thought 'take on empty stomach' meant 'don't eat breakfast'-so he skipped it for 3 days and his stomach started bleeding
it wasn't the pill
it was the silence
we didn't ask
we assumed
and that's the real killer
not the medicine
the not asking
i take my meds with a beer and call it a day
if it makes me feel better who cares what the label says
also i spelled 'pharmacist' wrong on my last prescription
they still gave it to me lol
you dont need to read all that stuff
just look for the big letters
if it says dont crush then dont crush
if it says refrigerate then put it in the fridge
thats it
I truly believe that every person deserves to understand their medication without needing a degree in medical decoding. If we can make labels clearer, offer translations, and encourage conversations-instead of just handing out paper-we can prevent so much suffering. Ask questions. Share what you learn. We’re all in this together.
Write a comment