When a child or adult starts taking ADHD stimulants like Ritalin, Adderall, or Vyvanse, the goal is clear: focus improves, impulsivity drops, and daily life gets easier. But behind that improvement is a quiet conversation many families don’t know they’re having-with their heart and their sleep. These medications work by boosting dopamine and norepinephrine in the brain, and that same surge affects the rest of the body. The result? Small but real changes in heart rate and blood pressure, and often, trouble falling asleep. The question isn’t whether these side effects happen-it’s how to recognize them, manage them, and decide if the benefits still outweigh the risks.
How Stimulants Affect Your Heart
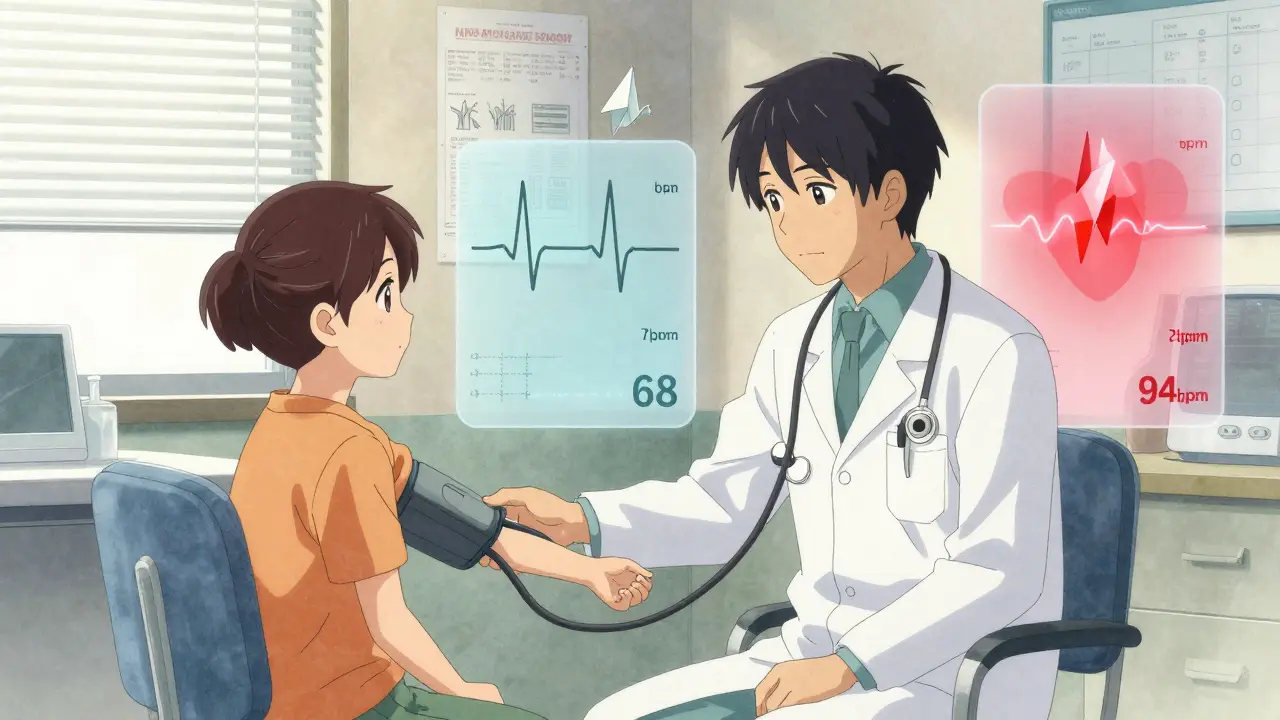
Stimulants don’t just sharpen focus-they slightly speed up your heart and nudge your blood pressure higher. It’s not dramatic, but it’s measurable. A 2025 study from the University of Southampton, the largest of its kind, found that after weeks of use, stimulants raised systolic blood pressure by 1 to 4 mmHg on average and increased heart rate by 1 to 2 beats per minute. That might sound tiny, but even small, sustained changes add up over time. The FDA confirmed this pattern across all major ADHD medications: methylphenidate, amphetamine, and even non-stimulants like atomoxetine. What surprises many doctors is that non-stimulants aren’t safer for the heart. In fact, the same study showed no meaningful difference in heart rate or blood pressure changes between stimulants and non-stimulants. The exception? Guanfacine. It actually lowers both. Long-term risks are more concerning. A 14-year study published in JAMA Psychiatry in 2024 found that people who took stimulants for ADHD had a 17% higher risk of developing cardiovascular disease-especially high blood pressure and artery problems. The risk grew with how long and how much they took, especially in the first three years. Another 2024 study from the American College of Cardiology found that young adults on stimulants were 17% more likely to develop cardiomyopathy after one year, and 57% more likely after eight years. But here’s the critical detail: the absolute risk remains very low. For every 1,000 people taking these meds, fewer than one might develop a serious heart issue because of them. The mechanism isn’t just about speed. Stimulants can cause blood vessels to tighten, trigger inflammation in artery walls, and, in rare cases, lengthen the QT interval on an ECG-a condition that can lead to dangerous heart rhythms. People with inherited Long QT Syndrome are at higher risk, but even then, the data isn’t black and white. Some studies show increased fainting episodes; others show no events at all. That’s why experts now say: don’t assume it’s unsafe. Do a careful check.Who Needs Extra Caution?
Not everyone needs an ECG before starting stimulants. The American Academy of Pediatrics says no to routine heart screenings, and most cardiologists agree. But certain red flags mean you should pause and talk to a doctor:- Personal or family history of sudden cardiac death before age 50
- Known heart defects, arrhythmias, or cardiomyopathy
- Unexplained fainting or chest pain during exercise
- High blood pressure already diagnosed
- Long QT Syndrome or a relative with it
Sleep Problems: The Silent Side Effect
If your child is wide awake at 11 p.m. after taking Adderall at 8 a.m., you’re not alone. About 30 to 50% of people experience trouble falling asleep when they first start stimulants. It’s not always the medication still being active-it’s the brain staying in high alert. Even extended-release pills that last 10 to 12 hours can interfere with sleep onset hours after the last dose. Studies show stimulant users take 15 to 30 minutes longer to fall asleep than those on placebo. The good news? For most, this fades after a few weeks as the body adjusts. But for others, it sticks around. That’s when you need to adjust the plan. Here’s what works:- Take the last dose earlier-by 3 p.m. at the latest
- Switch from extended-release to short-acting if you can split the dose
- Try melatonin: 0.5 to 5 mg, 1 to 2 hours before bed
- Build a wind-down routine: dim lights, no screens, quiet reading

What’s Safer? Stimulants vs. Non-Stimulants
Many assume non-stimulants are gentler on the heart. The data says otherwise. Atomoxetine and viloxazine raise heart rate and blood pressure just as much as Adderall or Ritalin. Guanfacine is the outlier-it lowers both. So if your main concern is cardiovascular strain, guanfacine might be the best non-stimulant choice. But if sleep is the bigger issue, atomoxetine often wins. It doesn’t cause the same kind of jittery wakefulness. It can make you tired at first, but that usually passes. And it doesn’t carry the same abuse potential as stimulants. There’s no perfect drug. The right choice depends on what matters most to you: focus, sleep, heart safety, or ease of use. That’s why treatment isn’t one-size-fits-all.Monitoring Is Key-But Don’t Fear the Medication
The biggest mistake? Avoiding stimulants out of fear. The benefits are real. Up to 80% of people with ADHD see major improvement. Kids do better in school. Adults hold jobs longer. Relationships improve. The American Heart Association used to push for ECGs before every prescription. Now, they say: focus on history and symptoms. Here’s what the latest guidelines recommend:- Take a full cardiac and sleep history before starting
- Check blood pressure and heart rate before and every 3-6 months
- Start low and go slow: begin with 5 mg of methylphenidate, increase by 5-10 mg weekly
- Watch for new chest pain, dizziness, fainting, or extreme insomnia
- Don’t skip follow-ups just because the child seems fine
What to Do Next
If you’re considering stimulants:- Ask your doctor for a baseline blood pressure and heart rate reading.
- Write down any family history of heart problems or sudden death.
- Track sleep patterns for the first two weeks-note when you fall asleep and how rested you feel.
- Don’t assume side effects mean the drug isn’t working. Give it time, but don’t ignore red flags.
- If sleep stays bad after 4 weeks, talk about switching formulations or adding melatonin.
- If heart rate stays above 100 bpm at rest, or blood pressure climbs above 140/90, get it checked.
- Check your last blood pressure reading. If it’s been over a year, schedule a visit.
- Ask your provider if your dose is still the right one-sometimes higher doses aren’t needed.
- Try moving your last dose earlier by 30 minutes each week until sleep improves.
- Keep a simple log: date, dose, heart rate (if you have a monitor), sleep time.
Do ADHD stimulants cause heart attacks?
Heart attacks from ADHD stimulants are extremely rare. While studies show a small increased risk of cardiovascular disease over many years, the absolute risk is low-less than 1 in 1,000 people per year. Most cases occur in those with pre-existing heart conditions or genetic risks. For healthy individuals, the risk is minimal compared to the benefits of improved focus and function.
Can I take melatonin with ADHD medication?
Yes, melatonin is commonly used alongside ADHD stimulants to help with sleep. A dose of 0.5 to 5 mg, taken 1 to 2 hours before bedtime, can help reduce sleep onset delay. It’s generally safe for short- and long-term use in children and adults. Always start low and check with your doctor if you’re on other medications.
Are non-stimulant ADHD meds safer for the heart?
Not necessarily. Atomoxetine and viloxazine raise heart rate and blood pressure just like stimulants. The only non-stimulant that lowers both is guanfacine. So if heart health is your top concern, guanfacine may be a better choice than other non-stimulants. But all ADHD medications require monitoring-none are risk-free.
How long do sleep problems last with ADHD meds?
For most people, sleep issues improve within 2 to 6 weeks as the body adjusts. If trouble sleeping continues beyond that, it’s likely due to timing or dose. Moving the last dose earlier, lowering the dose, or adding melatonin often helps. If sleep doesn’t improve after 4 weeks, talk to your doctor about switching medications.
Should my child get an ECG before starting ADHD medication?
Routine ECGs are not recommended for healthy children by the American Academy of Pediatrics or the American Academy of Neurology. But if there’s a family history of sudden cardiac death, unexplained fainting, or known heart rhythm problems, a cardiology evaluation and ECG are advised. The focus should be on personal and family medical history-not blanket screening.
15 Comments
I started my kid on Vyvanse last year. Sleep was a nightmare at first. We moved the dose to 7:30 a.m. and added 1mg melatonin. Now they’re asleep by 9:30. No big deal.
The data clearly shows that the absolute risk of cardiovascular events remains extremely low. Baseline monitoring and periodic checks are sufficient. Avoiding treatment due to fear is more harmful than the medication itself.
So you’re saying it’s fine to give a 9-year-old a drug that raises blood pressure just because ‘80% of kids do better in school’? What about the ones who don’t?
MY SON COULDNT SLEEP FOR WEEKS. I THOUGHT HE WAS BEING A BRAT. THEN WE TRIED MELATONIN. HE CRIED WHEN HE WOKE UP ON TIME. THIS CHANGED EVERYTHING.
I mean… like… it’s not that the meds are bad… it’s that we’ve… uh… normalized chemical… intervention… for… behavioral… differences? I just… wonder… if… we’re… missing… something… deeper?
Risk-benefit analysis must be individualized. The statistical risk is negligible. The functional gain is profound. Monitoring is the standard, not the exception.
To every parent scared of side effects: you’re not alone. But your child’s ability to focus, finish homework, and feel proud of themselves? That’s worth the small adjustments. You’ve got this.
I’ve seen this play out in two cultures. In the U.S., there’s fear of medication. In Nigeria, there’s fear of diagnosis. Both miss the point: ADHD is neurobiological. Treatment should be thoughtful, not ideological.
my niece got on adderall and her teacher said she was ‘a different kid’-like, she raised her hand for the first time. we didn’t know she was so quiet because she couldn’t focus. melatonin helped the sleep thing. no regrets.
The pharmacokinetic profile of extended-release stimulants exhibits a delayed peak plasma concentration, which correlates with prolonged sympathetic activation. This explains the circadian disruption observed in 30–50% of patients. Pharmacodynamic adaptation typically occurs within 14–42 days.
They’re just pushing drugs on kids because schools can’t handle them. You think a 7-year-old needs a stimulant? No. They need structure. Love. Discipline. Not chemistry.
I’m a nurse. I’ve seen this a hundred times. The biggest mistake? Waiting until the kid is failing everything to act. Baseline vitals, then track sleep. If it’s not working after 4 weeks, adjust-not panic.
I appreciate how this post emphasizes monitoring over fear. My brother was diagnosed at 16. He took methylphenidate for six years. His BP stayed normal. He graduated college. He’s now a software engineer. The risks were real-but manageable.
In Nigeria, we don’t even have access to these meds. My cousin with ADHD dropped out of school. No one knew what was wrong. I’m glad you’re talking about this. But please remember not everyone has a doctor to check BP.
This is a pharmaceutical industry propaganda piece. They profit from lifelong dependence. Wake up. ADHD isn’t a disease-it’s a personality trait they’re medicalizing to sell pills.
Write a comment