Every time you pick up a prescription, you’re handed a small piece of paper that could save your life-or hurt you if you don’t understand it. That little label isn’t just a receipt. It’s a safety map. And most people skip right over it.
Think about it: you’ve got a bottle of pills, maybe a liquid, maybe a patch. The label has names you don’t recognize, numbers that look like codes, tiny words crammed together. You’re tired. You’re worried. You just want to get home. But if you don’t read that label, you’re gambling with your health. Medication errors send over 1.5 million people to the emergency room every year in the U.S. And half of those mistakes happen because patients didn’t understand what the label said.
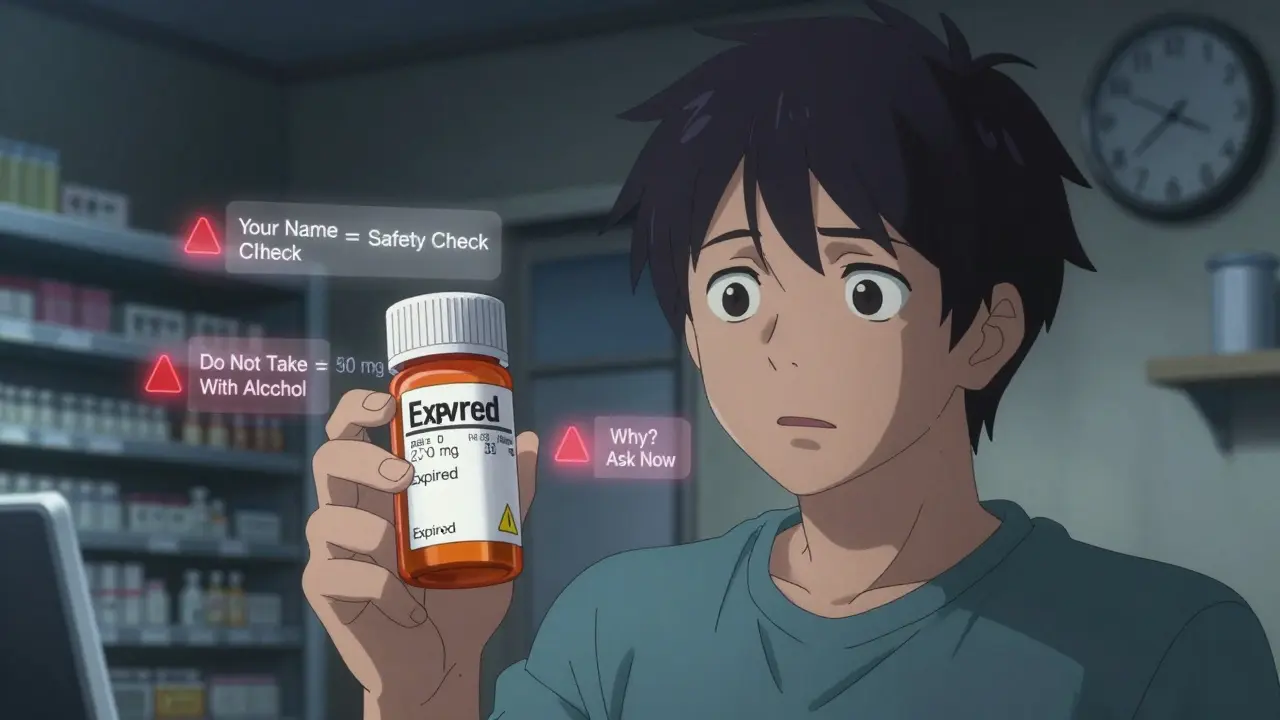
Your Name Is on There for a Reason
Look at the very top of the label. There’s your full name. It seems obvious, right? But this isn’t just for show. Pharmacists fill hundreds of prescriptions a day. Some drugs look almost identical. One wrong pill can cause a stroke, an overdose, or worse. In 2022, a woman in Ohio took someone else’s blood pressure medicine because her name was misspelled on the label. She ended up in the hospital. That’s why your name is printed in large, bold letters. Always check it. If it’s wrong, don’t take the medicine. Call the pharmacy right away.
Brand Name vs. Generic Name
You’ll see two names for your medication. The first is the brand name-like Abstral. That’s what the drug company calls it. The second is the generic name-fentanyl. That’s the actual medicine inside. Generic names are the same no matter who makes the drug. Brand names change depending on the company. If your doctor says you need fentanyl, but the label says Abstral, that’s okay. It’s the same thing. But if you’re told you’re getting lisinopril and the label says Zestril, you’re still getting the right drug. Knowing the difference helps you avoid confusion if you switch pharmacies or get a refill from a different place.
Dosage: What Each Pill or Drop Actually Contains
Look for a number followed by a unit-like 10 mg, 500 mcg, or 15 mL. That’s the strength. It tells you how much active medicine is in each pill, drop, or spoonful. A 10 mg tablet of metoprolol is not the same as a 50 mg tablet. Taking the wrong strength can be dangerous. If your doctor changes your dose, the label should change too. Don’t assume your old bottle is still right. Always compare the new label to what your doctor told you. If the number doesn’t match, call the pharmacy. They made a mistake.
How and When to Take It
This is the most important part. It tells you how often to take the medicine and under what conditions. It might say: “Take one tablet by mouth every 12 hours.” Or: “Take with food.” Or: “Take on an empty stomach.” Some meds need to be taken at the same time every day. Others need to be spaced out. Missing a dose or taking it too close to another can cause side effects or make the drug useless. If it says “as needed,” that means you only take it when you feel the symptom-like pain or nausea. Don’t take it just because you have the pill. And never take more than the label says, even if you don’t feel better.
Expiration Date: Don’t Use Old Medicine
That date on the label isn’t a suggestion. It’s a deadline. After that date, the medicine might not work as well. In some cases, it can break down into harmful substances. Most prescriptions expire 12 to 18 months after the pharmacy fills them. Some, like insulin or liquid antibiotics, expire much faster-even within 14 days once opened. Never take expired medicine. If you’re unsure, bring the bottle to your pharmacy. They’ll tell you if it’s still safe. And if you’ve had the same bottle for over a year, it’s probably time to get a new one.
The Rx Number and Pharmacy Info
The Rx number is like a fingerprint for your prescription. It’s how the pharmacy tracks your refill requests. If you call in for a refill and they ask for your Rx number, that’s why. It’s also how they know which doctor wrote the script. The pharmacy’s name, phone number, and address are right there on the label. Use them. If you have questions-about side effects, interactions, or how to take it-call the pharmacy. Pharmacists are trained to explain this stuff. Don’t wait until you feel sick to ask. And if you see your doctor’s name on the label, that’s your prescriber. If you need to change doctors or ask about alternatives, that’s who to contact.
What the Pill Looks Like
Some labels include a short description: “white, round, film-coated tablet.” Or: “clear, colorless liquid.” This helps you spot if something’s wrong. Say you get a refill and the pill looks different. It’s now blue instead of white. Or it has a different imprint. That doesn’t always mean it’s wrong-manufacturers change packaging. But it’s a red flag. Compare it to your old bottle. If it looks off, call the pharmacy. They might have given you a different brand or a mistake. Never swallow a pill that doesn’t match what you’re used to unless you’ve confirmed it’s safe.
The NDC Number: The Drug’s Unique ID
You’ll see a 10- or 11-digit number, usually near the bottom. That’s the National Drug Code (NDC). It’s like a barcode for your medicine. It tells you exactly who made it, what the drug is, and how it’s packaged. This number is used by insurance companies, hospitals, and the FDA to track prescriptions. You don’t need to memorize it. But if you’re ever asked for it-like when filing a claim or reporting a side effect-you’ll know where to find it.
Storage Instructions: Keep It Safe
Some meds need to be kept cold. Others must stay dry. If the label says “store at room temperature,” keep it in a cabinet-not the bathroom where steam and heat can ruin it. If it says “refrigerate,” put it in the fridge. Don’t freeze it unless it says so. Some insulin pens, for example, can’t be frozen. If you’re traveling, ask your pharmacist how to store your meds safely. Heat and moisture can make your medicine weak or dangerous.
Warnings: The Red Flags
This section is short but critical. It might say: “Do not take if you have liver disease.” Or: “May cause drowsiness-do not drive.” Or: “Avoid alcohol.” These aren’t suggestions. They’re rules. Ignoring them can lead to serious harm. For example, mixing certain painkillers with alcohol can cause liver failure. Taking blood thinners with certain supplements can cause dangerous bleeding. If you see a warning you don’t understand, ask. Don’t guess. Your life might depend on it.
Why You’re Taking It: The Missing Piece
Here’s something most labels still don’t say: why you’re taking this medicine. Is it for high blood pressure? For anxiety? For an infection? The FDA says this should be on every label. And experts say it cuts medication errors by more than half. If your label doesn’t say it, ask your pharmacist. Write it down yourself. “I’m taking metformin for diabetes” is way safer than “I’m taking metformin because the doctor gave it to me.” If you don’t know why you’re taking a drug, you’re more likely to stop it when you feel fine-even if you still need it.
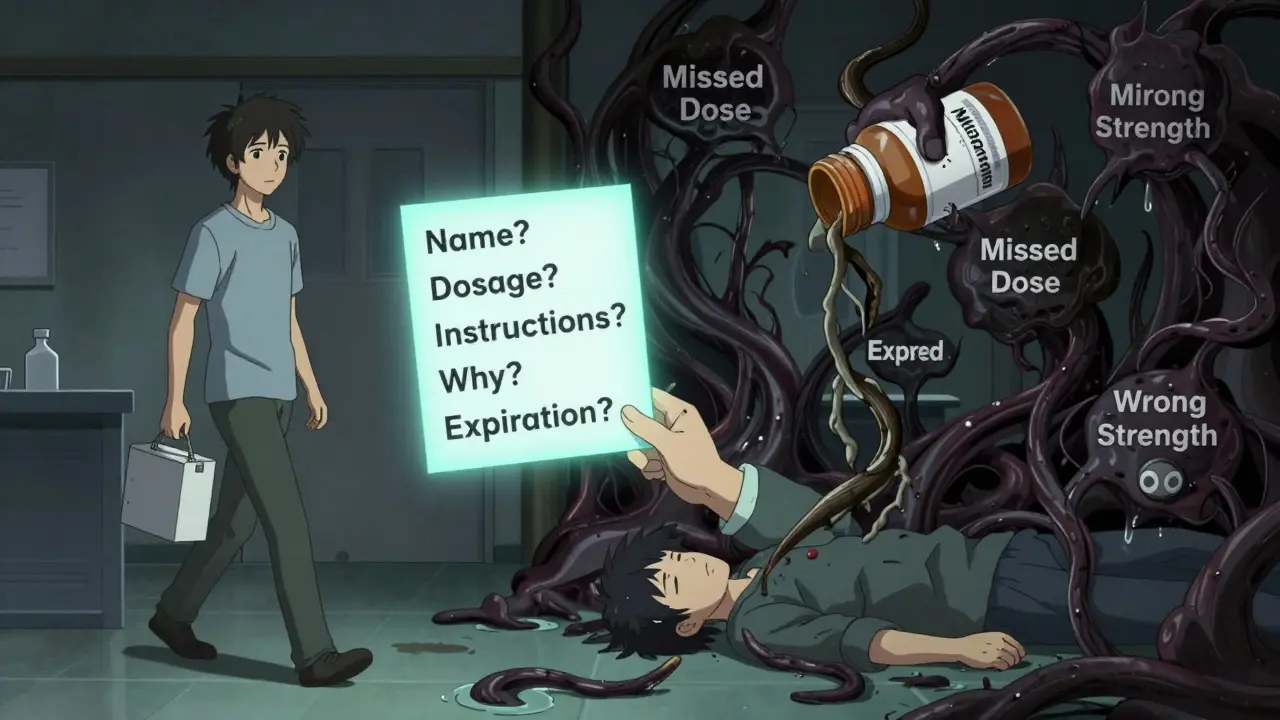
What to Do When You’re Confused
There are five questions every patient should ask every time they get a new prescription:
- What is the name of this medicine, and what is it for?
- How and when do I take it?
- What if I miss a dose?
- What side effects should I watch for?
- Will this interact with anything else I’m taking?
Some pharmacies offer a “teach-back” system. They’ll ask you to repeat the instructions in your own words. If you can’t, they’ll explain again. That’s not annoying-it’s lifesaving. Studies show patients who use this method are 28% more likely to take their meds correctly.
What’s Changing Soon
By 2025, the U.S. Pharmacopeia plans to require every prescription label to include the reason you’re taking the drug. That’s a big deal. Right now, only about 38% of pharmacies do it voluntarily. But once it’s mandatory, mistakes will drop. The FDA is also pushing for pictograms-simple icons showing how to take a pill or when to avoid food. These help people who struggle to read. And they’re already working in places like California and Massachusetts. If your label starts showing little pictures, don’t ignore them. They’re designed to help you, not confuse you.
Final Check Before You Leave the Pharmacy
Before you walk out, do a quick five-point review:
- Is your name correct?
- Does the medicine name match what your doctor told you?
- Is the dosage number right?
- Do you understand the instructions?
- Is the expiration date still good?
If anything feels off, stop. Ask. Don’t be shy. Pharmacists expect these questions. They’ve seen too many people hurt because they didn’t speak up.
12 Comments
I used to ignore labels too until my grandma nearly took someone else's blood thinner. Now I check every single thing - name, dosage, expiration. It’s not paranoia, it’s survival. That woman in Ohio? Could’ve been my mom. Always verify. Always.
Why the hell are we even talking about this? You think the government cares if you live or die? They print labels so you think you’re in control. Meanwhile, Big Pharma’s laughing all the way to the bank. You’re being manipulated. Read the fine print? Nah. Read the receipts - the real ones.
While the article presents a commendable overview of prescription label literacy, it fails to address the systemic underfunding of pharmacist education initiatives in rural communities. The NDC code, while standardized, is often misinterpreted even by clinical staff due to inconsistent database integration. Moreover, the absence of mandatory multilingual labeling in high-immigration regions constitutes a public health liability. The FDA’s 2025 initiative is a step, but insufficient without enforcement.
They’re putting a reason on the label? Yeah right. That’s just the first step before they start tracking your pills with microchips. Next thing you know, your insulin will beep when you skip a dose and send your data to the insurance company. They don’t care if you live - they care if you’re compliant. This isn’t safety. It’s surveillance.
This is the kind of post that should be mandatory reading in every high school health class. Seriously. We teach kids how to do algebra but not how to read a pill bottle? That’s insane. The five questions at the end? Print them on a sticky note. Put one on your fridge. Your future self will thank you.
Wow. What a touching PSA. Did you write this for your mom’s birthday? Or is this your new career as a pharmacy pamphlet poet? Let me guess - you also brush your teeth with organic Himalayan salt and meditate with crystals. Cute. The label doesn’t need to say why you’re taking it. You’re an adult. Figure it out. Or don’t. Your funeral will be cheaper without the lawsuit.
I’ve been on 17 different meds in the last 5 years. I’ve seen pills change color, size, shape, even taste. I’ve had pharmacists hand me something that looked like a child’s toy. One time I took a pill that made my tongue swell. I didn’t say anything because I thought I was imagining it. I almost died. Don’t be like me. Ask. Always ask. Even if you feel stupid. Your life isn’t a test of courage - it’s a test of curiosity.
My aunt just got her first prescription last week. She didn’t know what ‘QID’ meant. I showed her how to Google it. She said, ‘Why don’t they just say four times a day?’ I didn’t have an answer. Maybe the system’s broken, not the patient.
Oh sweet baby Jesus, the ‘why’ is missing? Of course it is. Because if you knew why you were taking that antidepressant, you’d have to admit you’re not okay. And that’s too much for Big Pharma. They’d rather you just swallow the little blue lie and keep scrolling. But hey - at least your label has a barcode. That’s progress, right?
Reading this made me cry. Not because it’s sad - because it’s so simple. We’re drowning in complexity, but the solution is just… asking. Just saying, ‘Can you explain this?’ Like you’re talking to a friend. Not a robot. Not a corporation. A human. That’s all it takes.
Check the name. Check the dose. Ask why. Done.
Every time I pick up a script, I read it like a contract - because it is. I don’t trust the system. But I trust myself to ask. And I’ve learned that pharmacists? Most of them want to help. They’re just swamped. So I bring coffee. And I say thank you. Small things. Big difference.
Write a comment