Anaphylaxis Symptom Checker
Based on CDC's ABCD recognition method for medication-induced anaphylaxis. If two or more symptoms appear within minutes of taking a drug, act immediately.
A - Airway
B - Breathing
C - Circulation
D - Dermatologic
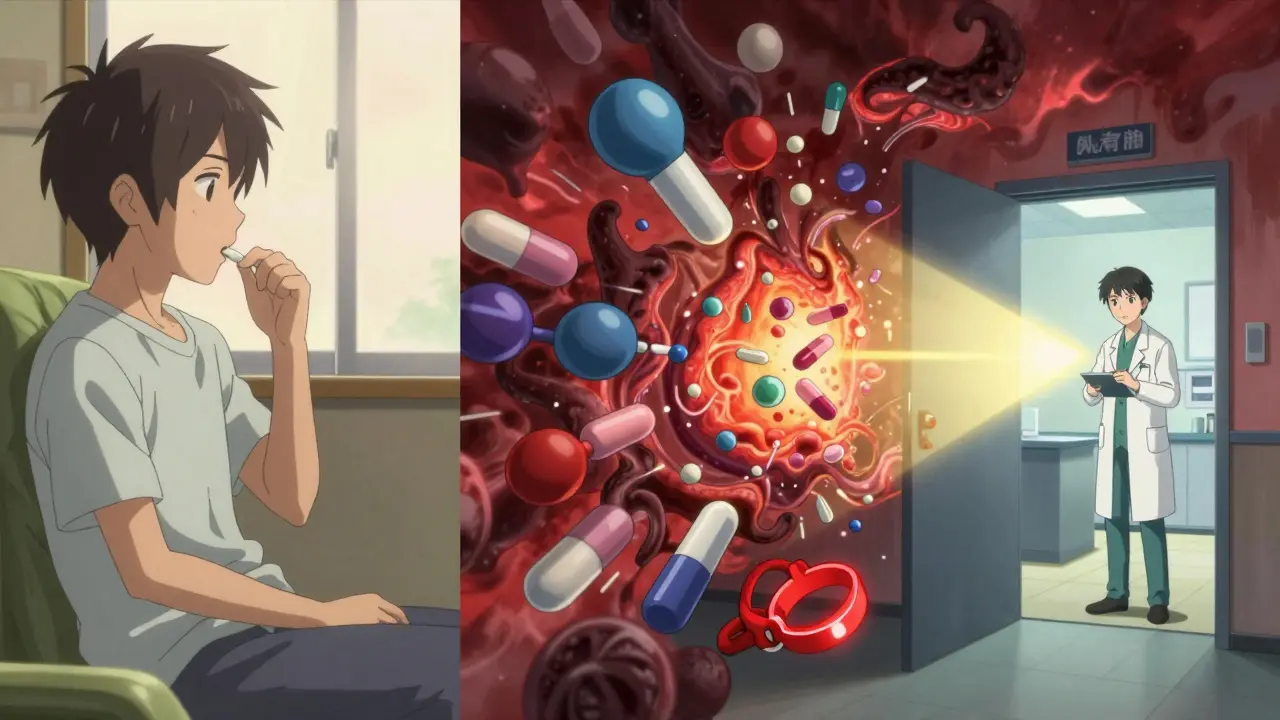
Medications save lives-but for some people, the very drugs meant to heal can trigger a sudden, life-threatening reaction. This is anaphylaxis, a severe, whole-body allergic response that can turn minutes into a fight for survival. Unlike a mild rash or itchy eyes, anaphylaxis strikes fast, hits multiple systems at once, and demands immediate action. And among all triggers, medications are one of the most common culprits in hospitals, clinics, and even at home.
What Happens During a Medication-Induced Anaphylaxis?
Anaphylaxis isn’t just an allergy-it’s a system-wide emergency. When a person reacts to a medication their body sees as dangerous, immune cells called mast cells and basophils explode with chemicals like histamine and tryptase. These chemicals cause blood vessels to leak, airways to tighten, and blood pressure to crash. The result? A cascade of symptoms that can escalate from mild to deadly in under 30 minutes.
According to the American Academy of Allergy, Asthma & Immunology (AAAAI), anaphylaxis is likely if any one of three criteria is met:
- Sudden skin or mucosal symptoms (hives, swelling, flushing) plus trouble breathing or low blood pressure
- Two or more body systems affected-like skin, lungs, gut, or heart-after taking a drug
- Low blood pressure alone after exposure to a known allergen
Medication-induced reactions often hit harder than food-triggered ones. A 2023 study in the journal Allergy found that 58% of drug-induced cases involved dangerously low blood pressure, compared to 39% for food. Respiratory distress-wheezing, throat tightness, gasping-was also more common. And while food reactions often start with vomiting or stomach cramps, drug reactions more frequently begin with dizziness, chest tightness, or a sense of impending doom.
Which Medications Cause the Most Reactions?
Not all drugs are created equal when it comes to triggering anaphylaxis. Antibiotics lead the list, making up nearly 70% of all medication-related cases. Penicillin and its relatives (like amoxicillin) account for 70-80% of those antibiotic reactions. But other drugs are just as dangerous:
- NSAIDs (like ibuprofen or aspirin): Cause 15% of cases. These aren’t always IgE-mediated-they can trigger reactions through other immune pathways.
- Monoclonal antibodies (rituximab, cetuximab): Used in cancer and autoimmune diseases. These have a high risk, especially during the first infusion.
- Chemotherapy agents (especially platinum-based drugs like cisplatin): Trigger reactions in about 4% of cases.
- IV contrast dye (used in CT scans): Often mistaken for anaphylaxis, but true allergic reactions are rare-most are non-allergic “contrast reactions.”
Even common over-the-counter drugs like acetaminophen can cause reactions in rare cases. The key isn’t just the drug class-it’s the individual’s history. A person who had a reaction once is far more likely to react again, even to a small dose.
Why Are These Reactions So Dangerous?
The biggest danger isn’t the reaction itself-it’s the delay in recognizing it.
In hospitals, symptoms like low blood pressure or wheezing are often blamed on anesthesia, infection, or anxiety. A 2022 study in JAMA Internal Medicine found that 41.7% of medication-induced anaphylaxis cases were initially misdiagnosed. One ER doctor in Massachusetts described a patient who developed hypotension after a CT scan. Staff thought it was a vasovagal episode-until the patient started struggling to breathe. Only then did they realize: this was anaphylaxis. Epinephrine reversed it in four minutes.
Delays cost lives. The Merck Manual reports that 78.3% of fatal cases involved delayed or missed epinephrine. In one chilling statistic: if epinephrine is given more than 30 minutes after symptoms start, the risk of death triples. And shockingly, 34.2% of people who died from anaphylaxis never received epinephrine at all.

How to Recognize It Fast: The ABCD Rule
You don’t need to be a doctor to spot anaphylaxis. Use the ABCD mnemonic, recommended by the CDC:
- Airway: Is the person’s throat swelling? Are they hoarse or struggling to speak?
- Breathing: Are they wheezing? Gasping? Is their oxygen level dropping?
- Circulation: Is their skin pale, cold, or clammy? Are they dizzy, fainting, or have a weak pulse?
- Dermatologic: Are hives, redness, or swelling appearing-especially on the face, lips, or tongue?
If two or more of these show up within minutes of taking a medication, assume it’s anaphylaxis. Don’t wait. Don’t second-guess. Act.
Epinephrine Is the Only Lifesaver
There’s no substitute. Antihistamines like Benadryl? They help with itching, but they won’t stop a crashing blood pressure or closing airway. Steroids? They reduce inflammation later-but not now. Only epinephrine works fast enough.
The correct dose for adults is 0.3-0.5 mg injected into the outer thigh. It’s not a shot in the arm or the butt. The thigh muscle absorbs it fastest. Auto-injectors (like EpiPen or Auvi-Q) are designed for this. If you’re unsure how to use one, practice with a trainer device. Hospitals and clinics should have multiple epinephrine kits on hand-not just one.
Studies show that 87.2% of successful outcomes are tied to proper injection technique. A 2022 trial at Baylor College of Medicine found that after training ER staff with simulations, epinephrine use jumped from 48% to nearly 90% in under six months.
What Happens After the Reaction?
Even if symptoms improve after epinephrine, you’re not out of danger. Up to 20% of cases have a second wave-called biphasic anaphylaxis-hours later. That’s why everyone who has an anaphylactic reaction must be observed for at least 4-6 hours in a medical setting.
And here’s the heartbreaking truth: 52.6% of patients who survive medication-induced anaphylaxis leave the hospital without a prescription for an epinephrine auto-injector. That’s not just a gap in care-it’s a death sentence waiting to happen. If you’ve had one reaction, you’re at higher risk for another. You need the tool to survive the next one.
Patients should also be referred to an allergist. Skin testing or blood tests can help identify the specific drug culprit. In some cases, desensitization protocols can allow safe future use-especially for essential drugs like chemotherapy or antibiotics with no alternatives.
Prevention Is Possible
The good news? Most medication-induced anaphylaxis is preventable.
Johns Hopkins Hospital cut their anaphylaxis incidents by 47% in just two years by implementing an allergy alert system that flags drug allergies in electronic records. Before, 63% of errors happened because the patient’s allergy history was missing or unclear.
Now, the Joint Commission requires all accredited hospitals to have anaphylaxis recognition protocols in place as of January 1, 2024. The FDA has also mandated stronger warning labels on biologic drugs. And new tools are emerging-like the AllergoCheck IgE Rapid Test, approved in 2023, which can confirm penicillin allergy in minutes.
But technology alone won’t fix this. Training, vigilance, and clear communication between patients and providers are still the backbone of prevention. If you’ve ever had a reaction, make sure your doctor, pharmacist, and ER team know. Carry a medical alert card. Update your records. And if you’re prescribed a new drug, ask: “Could this cause anaphylaxis?”
Final Reality Check
Anaphylaxis from medications is not rare. It’s not random. It’s predictable-and preventable. Every year, over 38,000 people in the U.S. alone show up to emergency rooms because of it. The cost? Over $70 million in direct care. But behind those numbers are real people-patients who almost died because no one recognized the signs.
The next time someone gets a shot, starts an IV, or swallows a pill, ask yourself: Could this be the moment? If you see sudden swelling, trouble breathing, or a sudden drop in energy-don’t wait. Don’t assume it’s anxiety. Don’t wait for a doctor. Give epinephrine. Call for help. Save a life.
Can you have anaphylaxis without hives?
Yes. While hives and skin symptoms are common, up to 20% of anaphylaxis cases occur without any visible rash. This is especially true with medication-induced reactions, where low blood pressure, wheezing, or sudden dizziness may be the only signs. Never rule out anaphylaxis just because there’s no rash.
Is anaphylaxis always immediate after taking a drug?
Most reactions happen within 5 to 30 minutes, especially with IV drugs. But delayed reactions can occur up to 6 hours later, particularly with oral medications like antibiotics or NSAIDs. If you feel unusual symptoms hours after taking a drug, don’t ignore them-especially if you’ve had a reaction before.
Can you outgrow a medication allergy?
Sometimes, yes. Penicillin allergies, for example, can fade over time. About 80% of people who had a reaction 10 years ago will no longer test positive. But never assume you’re safe-always get tested by an allergist before reusing a drug you once reacted to.
What’s the difference between anaphylaxis and a side effect?
Side effects are predictable and common, like nausea from chemo or flushing from niacin. Anaphylaxis is unpredictable, rapid, and involves multiple organ systems. If symptoms include throat tightness, trouble breathing, dizziness, or a racing pulse right after taking a drug, it’s likely an allergic reaction-not just a side effect.
Why do some people react to drugs they’ve taken before?
The immune system can become sensitized after repeated exposure. The first time you take a drug, your body may not react. But after multiple doses, it can start recognizing it as a threat. That’s why a person can have a mild reaction once, then a severe one later-even if the dose is the same.

15 Comments
My sister had a reaction to amoxicillin last year. No hives, just dizziness and trouble breathing. We thought it was a virus until the ER doc said, 'This is anaphylaxis.' Now she carries two EpiPens. Don’t wait for the rash.
It’s scary how often this gets missed. Even in hospitals.
Oh great. Another ‘epinephrine is magic’ lecture. Meanwhile, 40% of people can’t afford the damn auto-injectors. But sure, let’s blame the patient for not having a $600 lifesaver they weren’t even warned to buy.
Real solution? Make it free. Not more bullet points.
I work in ER and saw a case where a guy got IV contrast and went into shock. Staff thought it was anxiety. Took 12 minutes to get epinephrine. He’s fine now but… damn. We need better training. Not just posters on the wall.
Also, typo: 'dose' not 'dose' - just saying.
It’s wild how much we’ve learned in the last decade. Back in the 90s, we’d just give Benadryl and hope. Now we know: no rash? Still anaphylaxis. Delayed? Still dangerous. Oral meds? Still deadly.
What gives me hope is how many nurses and EMTs are now trained to spot this in under 10 seconds. It’s not perfect, but we’re getting better. And that matters.
Thanks for writing this. It’s the kind of info that saves lives when no one’s looking.
Let’s be real - the whole system is a dumpster fire. We have pharmacists who can’t spell ‘anaphylaxis’ on the chart, doctors who think ‘it’s just a side effect,’ and patients who don’t even know they have a drug allergy because they were too scared to ask. And now we’re supposed to rely on a $600 plastic pen to save us? No.
It’s not about epinephrine. It’s about systemic failure. We need mandatory allergy documentation in all EHRs, standardized training for all frontline staff, and yes - government-funded auto-injectors. Not ‘here’s a pamphlet, good luck.’
And stop calling it ‘anaphylaxis.’ Call it what it is: a medical negligence crisis.
Why are we letting Big Pharma get away with this? They know these drugs are dangerous. They know the reactions are common. But they don’t warn you. They don’t test enough. And then they charge you $600 for the antidote.
This isn’t science. This is capitalism with a stethoscope.
Epinephrine should be on every corner like a fire extinguisher. Not locked in a cabinet while someone’s dying.
My cousin got anaphylaxis from a flu shot. No hives. Just passed out. They thought she was drunk. Took 20 minutes before someone checked her vitals. She’s okay now, but it broke me.
If you take meds, know the signs. If you work in healthcare, don’t assume. Ask. Listen. Act. It’s that simple.
I’m a nurse and I’ll tell you - the biggest problem isn’t the patients. It’s the paperwork. We have a 12-page form for allergies, but half the time it’s incomplete, outdated, or buried under 30 other tabs. One guy came in with a penicillin allergy… but his chart said ‘possible reaction, no confirmation.’ So we gave him amoxicillin. He went into shock. We got lucky he had his own EpiPen.
Technology isn’t the fix. People are. We need to talk to patients. Not just check boxes.
My dad had a reaction to IV contrast. No one knew he was allergic. He was fine after epinephrine, but we almost lost him.
Now he carries a card. I made it for him. Simple words. Big font. ‘Allergic to iodine contrast. Epinephrine needed.’
If you’ve had a reaction, do this. It’s not dramatic. It’s just smart.
I’ve had three reactions. First one, I thought I was having a panic attack. Second, I ignored it. Third, I used my EpiPen myself. I’m alive because I learned. Don’t wait to be brave. Be prepared.
It is, of course, profoundly lamentable that the American healthcare system has reached such a state of abysmal incompetence that the administration of a life-saving epinephrine injection - a procedure so rudimentary that it was first documented in 1901 - is now treated as if it requires a PhD in emergency medicine.
And yet, the FDA, in its infinite wisdom, has mandated labeling on biologics, while simultaneously failing to mandate universal, real-time allergy integration into EHRs - a glaring, indefensible oversight that betrays a fundamental failure of governance.
One might argue that this is not merely a medical issue, but a philosophical one: when do we cease to treat human life as a commodity, and begin to treat it as an inviolable right?
…I digress. The point is: penicillin allergy testing is underutilized. And that is tragic.
From India: we don’t have EpiPens everywhere. But we teach nurses to use ampules and syringes. Epinephrine 1:1000, 0.3 ml IM. Same result. Cheap. Effective.
Don’t wait for fancy pens. Learn the basics. It saves lives.
My uncle died from this. No one knew he was allergic to NSAIDs. He took ibuprofen for back pain. 10 minutes later, he was gone.
Now I carry an EpiPen. And I tell everyone I know: if you take meds, ask. If you see someone struggling, act.
❤️
While the article provides a comprehensive overview of anaphylaxis, it is worth noting that the term ‘biphasic reaction’ is sometimes misused in lay discourse. True biphasic anaphylaxis requires recurrence of symptoms after initial resolution, not merely delayed onset. The distinction is clinically significant, as management protocols differ.
Additionally, the assertion that ‘epinephrine is the only lifesaver’ is accurate, but the implication that antihistamines and corticosteroids are useless is misleading - they remain adjunctive therapies in preventing late-phase reactions.
Let me be perfectly clear: if you’re not carrying an EpiPen after one reaction, you are not just irresponsible - you are a danger to yourself and others. There is no excuse. Not cost. Not forgetfulness. Not ‘I didn’t think it would happen again.’
You think it’s dramatic? It’s not. It’s survival. And if you’re one of those people who say, ‘I’ll just go to the hospital,’ you’re one step away from being a statistic.
Wake up. Get the pen. Carry it. Use it. Don’t be a victim. Be prepared.
Write a comment