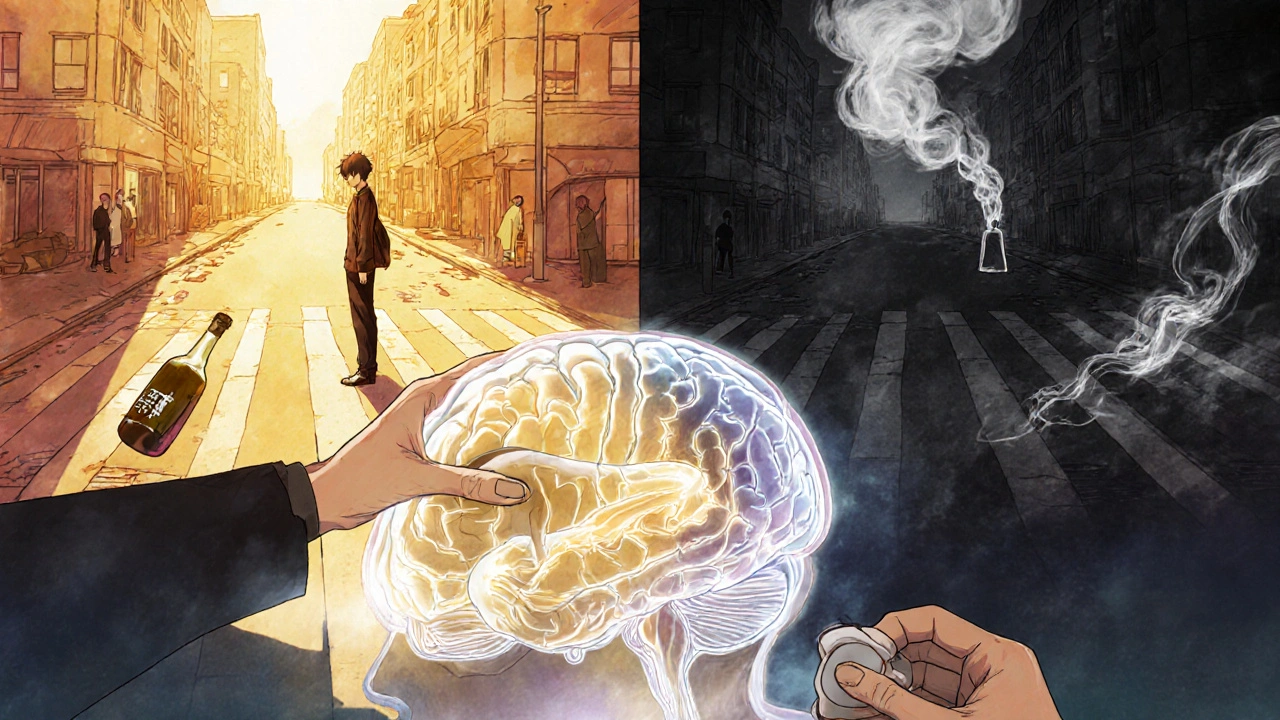
Chronic Alcohol Use Disorder isn’t just about drinking too much. It’s a medical condition where your brain and body become trapped in a cycle of dependence, even when alcohol is destroying your health, relationships, and life. It doesn’t happen overnight. It creeps in slowly-maybe starting with a drink after work, then a few more on weekends, then needing it just to feel normal. By the time someone realizes they can’t stop, the damage is often already deep.
How Alcohol Changes Your Brain and Body
Alcohol isn’t just a depressant-it rewires your brain. Over time, your brain starts relying on alcohol to function normally. When you stop drinking, your nervous system goes into overdrive. That’s why withdrawal isn’t just uncomfortable-it can be deadly. Symptoms like shaking, rapid heartbeat, confusion, and seizures aren’t signs of weakness. They’re proof your body has adapted to alcohol’s presence.
At the same time, your liver is taking a beating. About 90% of heavy drinkers develop fatty liver disease. It’s reversible-if you quit. But if drinking continues, it progresses to alcoholic hepatitis, where liver cells die from inflammation. Then comes cirrhosis: scar tissue replaces healthy liver tissue. Once cirrhosis sets in, your liver can’t filter toxins, produce proteins, or store energy properly. Some damage can heal after stopping, but not all. The longer you drink, the less chance you have of full recovery.
Organ Damage You Can’t Ignore
Your heart isn’t safe either. Heavy drinking raises your risk of high blood pressure by 16%, increases your chance of stroke by 34%, and makes atrial fibrillation-irregular heartbeat-40% more likely. These aren’t distant risks. They’re direct results of alcohol’s effect on your cardiovascular system.
Your pancreas gets inflamed. Your immune system weakens. You’re 2.7 times more likely to get pneumonia. Your stomach lining gets irritated, leading to ulcers and bleeding. Your bones thin out, increasing fracture risk. Even your skin changes-redness, puffiness, broken capillaries-often called "alcoholic face." It’s not just cosmetic. It’s a visible sign of internal damage.
And then there’s your brain. Long-term alcohol use shrinks brain tissue. Memory fails. Thinking slows. You might develop Wernicke’s encephalopathy-a severe brain disorder caused by vitamin B1 deficiency, which affects up to 80% of people with chronic AUD. Left untreated, it can lead to Korsakoff syndrome: permanent memory loss, confusion, and inability to form new memories.
Cancer Risk Is Real-and Preventable
Alcohol is a known carcinogen. The American Cancer Society says heavy drinkers have five times the risk of mouth and throat cancer. For every drink consumed daily, breast cancer risk increases by 12%. Liver cancer risk rises sharply with cirrhosis. Bowel cancer risk climbs too. There’s no safe level if you’re drinking regularly. The more you drink, the higher your risk. But the good news? Stopping can reduce that risk over time.
Mental Health and the Vicious Cycle
Many people turn to alcohol to cope with anxiety or depression. But alcohol makes both worse. It disrupts serotonin and dopamine levels. It worsens sleep. It fuels negative thoughts. What starts as self-medication becomes a trap. You drink to feel better. You feel worse. You drink again. It’s a loop that breaks relationships, jobs, and self-worth.
Studies show people with chronic AUD are more likely to experience homelessness, unemployment, and financial collapse. The cost isn’t just personal. In the U.S. alone, excessive drinking cost $249 billion in 2010-mostly from lost productivity, healthcare, and criminal justice expenses. And it’s not just about money. Alcohol contributes to nearly a third of all traffic deaths in the U.S. Every year, 3 million people worldwide die because of alcohol. That’s one death every 10 seconds.

What Treatment Actually Works
Treatment isn’t one-size-fits-all. It’s not about willpower. It’s about medical care.
First step: detoxification. If you’ve been drinking heavily for months or years, quitting cold turkey can be dangerous. Seizures and delirium tremens (DTs) can be fatal. Medical detox-done in a clinic or hospital-uses medications to safely manage withdrawal. This isn’t giving up. It’s preparing for recovery.
After detox, three FDA-approved medications help prevent relapse:
- Naltrexone blocks the pleasurable effects of alcohol, reducing cravings.
- Acamprosate helps stabilize brain chemistry after stopping.
- Disulfiram makes drinking unpleasant-causing nausea, flushing, and headaches if alcohol is consumed.
Medication alone isn’t enough. Therapy is critical. Cognitive Behavioral Therapy (CBT) helps you recognize triggers and build new habits. Studies show CBT reduces heavy drinking days by 60%. Motivational Enhancement Therapy helps people who feel stuck-ambivalent about quitting. It’s not about being told what to do. It’s about finding your own reason to change.
Support Systems Make a Difference
Alcoholics Anonymous (AA) has helped millions since 1935. Their 12-step program isn’t for everyone, but for many, the structure and peer support are life-saving. Their own data shows 27% of members stay abstinent after one year. Other groups like SMART Recovery offer science-based, non-spiritual alternatives. The key? Finding a community that keeps you accountable and reminds you you’re not alone.
New Treatments on the Horizon
Science is catching up. Transcranial Magnetic Stimulation (TMS)-a non-invasive brain stimulation technique-showed 50% abstinence rates in a 2022 study. Digital tools like the reSET app, approved by the FDA, help people track cravings and access therapy on their phone. In trials, users using reSET were more than twice as likely to stay sober compared to those without it.
The MATTERS study proved something simple but powerful: combining medication with therapy increases abstinence rates by 24% over either treatment alone. This isn’t experimental. It’s the new standard of care.
Why So Few Get Help
Despite all this, only 19.2% of the 14.5 million Americans with AUD get treatment. Why? Stigma. Fear. Lack of access. Many still see AUD as a moral failure, not a medical condition. Insurance doesn’t always cover it. Treatment centers are hard to find, especially outside big cities. And many people don’t realize they have a problem until it’s too late.
But recovery is possible-even after years of drinking. The liver can regenerate. The brain can heal. Relationships can be rebuilt. You don’t need to hit rock bottom to start healing. You just need to want to stop.
When to Seek Help
You don’t need to be an "alcoholic" to need help. If you:
- Drink more than you planned
- Feel guilty about your drinking
- Need alcohol to relax or sleep
- Have tried to quit but couldn’t
- Notice your health is declining
-then it’s time to talk to a doctor. No judgment. No shame. Just facts. AUD is treatable. And the sooner you act, the more of your life you can save.
Can you recover from liver damage caused by alcohol?
Yes, but it depends on how far the damage has gone. Fatty liver and mild inflammation can reverse completely within weeks or months of stopping alcohol. Alcoholic hepatitis can improve significantly if you quit early. But once cirrhosis develops-where scar tissue replaces healthy liver cells-the damage is often permanent. Even then, stopping alcohol can stop further damage and improve life expectancy. The key is early action.
Is alcohol use disorder the same as alcoholism?
Yes, but the term "alcoholism" is outdated. Today, doctors use "Alcohol Use Disorder" (AUD), which covers a spectrum from mild to severe. What people used to call "alcoholism" is now classified as severe AUD. The change was made to reduce stigma and recognize that addiction exists on a scale-not just as an all-or-nothing condition.
Can you drink again after treatment?
For most people with moderate to severe AUD, returning to any level of drinking leads to relapse. Recovery isn’t about moderation-it’s about abstinence. Some people with mild AUD may learn to control their drinking, but this is rare and risky. The safest path for long-term health is complete avoidance. Think of it like quitting smoking: you don’t go back to one cigarette.
How long does alcohol withdrawal last?
Withdrawal symptoms usually start 6-12 hours after the last drink. Peak symptoms occur between 24-72 hours. Most physical symptoms like shaking, nausea, and sweating fade within a week. But psychological symptoms-anxiety, insomnia, cravings-can last weeks or months. This is why ongoing therapy and support are essential. Medical supervision during detox reduces risks and makes the process safer.
Are medications for AUD just replacing one addiction with another?
No. Medications like naltrexone, acamprosate, and disulfiram don’t create addiction. They don’t produce euphoria. They work by reducing cravings or making drinking unpleasant. Think of them like insulin for diabetes-they correct a biological imbalance. These drugs are used for months or years under medical supervision, not as a quick fix. They’re tools to support recovery, not substitutes for alcohol.
What if I’m not ready to quit completely?
You don’t have to have all the answers right now. The NIAAA’s Rethinking Drinking guide helps people reduce their intake even if they’re not ready to stop entirely. Cutting back lowers your risk of liver disease, cancer, and accidents. But if you’re drinking heavily or experiencing withdrawal symptoms, reducing alone isn’t enough. Talk to a doctor. They can help you decide if moderation is safe-or if quitting is the only path forward.
What Comes Next
If you’re reading this and recognize yourself, don’t wait. The longer you delay, the more damage accumulates-and the harder recovery becomes. Start by talking to your doctor. Ask about screening for AUD. Ask about medications. Ask about therapy options. You don’t need to go it alone.
Recovery isn’t about perfection. It’s about progress. One day at a time. One choice at a time. And every choice not to drink is a step back toward your life.

11 Comments
They say alcoholism is a disease but look at the data bro its just weak people who cant handle life. Government and pharma want you hooked on meds like naltrexone so they can keep cashing in. I seen guys quit cold turkey in the army no problem. Why you think they dont tell you that?
Its all control. You dont need therapy you need discipline. Stop blaming the booze and start blaming yourself.
I really appreciate how detailed this is. I’ve watched someone I love go through this and the part about brain shrinkage and Wernicke’s really hit home. It’s not just about willpower - it’s biology. Thank you for explaining it without shame.
It is imperative to underscore that the statistical prevalence of alcohol-related mortality within the United States constitutes a public health exigency of the highest order. The conflation of medical science with populist narratives undermines the integrity of clinical practice. One must recognize that the FDA-approved pharmacotherapies referenced herein are not merely adjunctive - they are foundational to evidence-based recovery paradigms. To suggest otherwise is not only inaccurate, it is dangerously irresponsible.
Extremely well-articulated synthesis of the neurobiological, hepatological, and psychosocial dimensions of AUD. The MATTERS study findings are particularly compelling - the synergistic effect of pharmacotherapy and CBT demonstrates a robust effect size (Cohen’s d > 0.8) in sustained abstinence outcomes. The real challenge lies in scalability: access to integrated care remains fragmented, especially in rural and underserved communities. We need policy reform to mandate parity in insurance coverage for AUD treatment equivalent to other chronic conditions.
It’s funny how we call it a disorder when it’s really just the body screaming for balance. We live in a world that rewards numbness - alcohol is just the easiest tool to get there. The real question isn’t why people drink - it’s why we’ve built a society where so many feel they need to escape. Healing isn’t about quitting alcohol. It’s about learning how to be present without it.
OMG this is SO important!!! 🙌 I just read this and I’m crying because my cousin just went through detox and they gave her disulfiram and she said it felt like someone finally saw her. Like… she wasn’t a ‘bad person’ she was sick. 💔💉 The liver regenerates??? I didn’t know that!!! 🤯 I’m telling everyone I know. Also - TMS?? Like the brain zap thing?? That’s wild!! I’m researching this right now. #AlcoholIsNotAChoice #RecoveryIsPossible
Bro I was drinking 2 bottles of whiskey a day for 8 years. Liver enzymes through the roof. Doctors said I had 2 years if I didn’t stop. I did. No rehab. No AA. Just woke up one day and said ‘fuck this’. 4 years clean now. My skin looks like a different person. I can remember my kid’s birthday without a hangover. You don’t need meds. You don’t need therapy. You need to stop lying to yourself. One day at a time? Nah. One decision. One time. That’s it. The rest is just cleanup.
It’s not just about the alcohol - it’s about the silence that comes after. The way your hands shake when you try to hold your child. The way your partner stops asking if you’re okay because they already know the answer. I used to think recovery meant never drinking again - now I know it means learning how to sit with your own thoughts without running. And that? That’s the hardest part. But it’s worth it. So worth it.
This is exactly what people need to hear.
Let’s be real - this whole ‘AUD is a disease’ narrative is just woke propaganda to excuse bad behavior. In my country, we don’t coddle weakness. You drink too much? Then you’re weak. Period. Stop making excuses with brain scans and FDA approvals. Take responsibility. That’s what real men do. This country is falling apart because we’ve turned vice into a medical diagnosis.
So let me get this straight - you’re telling me the same people who told me to ‘just stop drinking’ for 10 years are now selling me a $200/month app that talks to me like a therapist? 😂
Thanks for the laugh. I’ll take the meds, the therapy, the TMS, and the damn app - because when you’re drowning, you don’t get to pick your life raft. Even if it’s a glittery one.
Write a comment